7. BHSA Components and Requirements
A. Behavioral Health Services and Supports
A.1 Behavioral Health Services and Supports Expenditure Guidelines
Counties are required to allocate 35 percent of their total local Behavioral Health Services Act (BHSA) allocations for Behavioral Health Services and Supports (BHSS).[1] BHSS categories include:
Children’s, Adult, and Older Adult Systems of Care
Outreach and Engagement
Workforce Education and Training
Capital Facilities and Technological Needs
Early Intervention Programs
Innovative Behavioral Health Pilots and Projects
Of the 35 percent of funds allocated to BHSS, counties are required to use 51 percent of funds for Early Intervention Programs, and of that, 51 percent of the funds for Early Intervention Programs must be used to serve BHSA eligible individuals who are 25 years of age and younger. Counties may, but are not required to, fund BHSS categories other than Early Intervention. Counties will be required to report on the amount of BHSS funds, planned expenditures in the Integrated Plan and actual expenditures in the Behavioral Health Outcomes, Accountability, and Transparency Report (BHOATR), apportioned to each BHSS category they choose to fund. Additional information on county allocation requirements can be found in Chapter 6, Section B.1.
Counties may include Innovative Behavioral Health Pilots and Projects across all BHSS categories. Additional information on Innovative Behavioral Health Pilots and Projects can be found below in Chapter 7, Section A.6.
Counties should maximize the use of other available sources of funding, including Medi- Cal, to provide BHSS services. However, counties are not required to exhaust these other funding sources before using BHSS funds. Additional information on requirements to maximize non-BHSA sources of funding can be found in Chapter 6, Section C.
Counties may use shared resources to advance multi-county BHSS projects. Each county will be expected to report on multi-county projects in their respective Integrated Plan.
A.2 Children’s, Adult, and Older Adult Systems of Care
Counties may use a portion of BHSS funds to provide Children’s, Adult, and Older Adult Systems of Care services, including substance use disorder services, to BHSA eligible and priority populations. System of care services are those pursuant to Part 4 for the Children’s System of Care and Part 3 for the Adult and Older Adult System of Care.[2] Additional information on BHSA eligible and priority populations can be found in Chapter 2, Section B.3.
Children’s, Adult, and Older Adult Systems of Care services funded under BHSS may not include Housing Interventions or services for individuals enrolled in a Full Service Partnership (FSP). Housing Interventions and FSP services should be funded under those components.
A.3 Outreach and Engagement
Counties may use a portion of BHSS funds for Outreach and Engagement (O&E). BHSS funds may be used for activities intended to reach, identify, and engage individuals, families, and communities in the behavioral health system and reduce disparities.
Counties may include evidence-based practices and community-defined evidence practices in the provision of activities.[3]
BHSS O&E activities involve broad engagement of unserved and underserved populations in the behavioral health system. These activities are distinct from those that may be funded as part of BHSS Early Intervention Programs, Housing Interventions, or FSP programs. County Early Intervention programs must include an outreach component, and counties may use FSP funding for outreach activities to enroll individuals in an FSP. Additionally, counties may utilize up to 7 percent of their Housing Intervention funds on identified Outreach and Engagement activities. O&E activities that are required as a part of as part of BHSS Early Intervention programs or FSP should be funded and tracked in county Integrated Plans (IPs) and BHOATRs as part of those programs, rather than under the BHSS O&E category. Additional information on BHSS Early Intervention can be found in Chapter 7, Section A.7 and additional information on FSPs can be found in Chapter 7, Section B.
BHSS funds may be used for O&E activities to engage individuals in housing interventions, if the county is not funding these activities under Housing Interventions . For example, BHSS funds may be used to conduct outreach to individuals in encampments to support connection to housing programs. Additional information on allowable uses of Housing Intervention funds can be found in Chapter 7, Section C.
When the county works in collaboration with other non-behavioral health community programs and/or services, only the costs directly associated with outreach and engagement activities to provide mental health and substance use treatment can be funded under the BHSS O&E category.
Examples of O&E activities that may be supported with BHSS funds include but are not limited to:
Outreach to and collaboration with individuals and entities that can help reach, identify, and engage individuals and communities in the behavioral health system, which may include but are not limited to:
Community-based organizations
Housing Agencies
Street medicine/field-based service providers
Harm reduction/syringe services programs
Community leaders
Schools
Early Care and Learning
Tribal communities
Primary care providers
Senior centers
Senior Housing (including affordable senior housing and other types of retirement communities, local Area Agencies on Aging, and the local Aging and Disability Resource Connections)
Hospitals (including emergency departments and behavioral health urgent care)
Federally Qualified Health Centers
Faith-based organizations
Outreach to directly reach and engage individuals who may benefit from behavioral health services and engagement to support and encourage ongoing participation of the eligible population in behavioral health treatment, such as:
Peer Support Services[4] including resource navigation.
Enhanced Community Health Worker services[5] under Behavioral Health Community-Based Organized Networks of Equitable Care and Treatment (BH-CONNECT), which include health navigation, health education, support and advocacy, and tailored preventive services for Medi-Cal members living with significant behavioral health needs.
Food, clothing, and other basic necessities, when the purpose is to engage unserved individuals and, when appropriate, their families in the behavioral health system. These services should support the ability to provide for the immediate needs of an individual.
Strategies to reduce ethnic, racial, gender-based, age-based, or other disparities, such as:
Engaging individuals, families, and credible messengers from priority communities to design and provide input on outreach strategies and messages so that they meet the unique needs of those populations.
Outreach to individuals through community sites that are natural gathering places for priority populations.
A.4 Workforce Education and Training
Counties may use a portion of BHSS funds for Workforce Education and Training (WET). County-operated and/or county-contracted providers that are employed or volunteer in the county behavioral health delivery system may participate in WET activities.
Counties should incorporate efforts to increase the racial, ethnic, and geographic diversity of the behavioral health workforce, including incorporating individuals with lived experience into the workforce, across all WET activities. BHSS funds for WET activities must be spent within ten years, after which unspent funds will be subject to reversion. All transfers into WET are irrevocable and cannot be transferred out of WET. Additional information on fiscal policies can be found in Chapter 6, Sections B.7 and B.8.
A.4.1 WET Alignment with Statewide Workforce Initiatives
WET activities must supplement, but not duplicate, funding available through other state-administered workforce initiatives, including the Behavioral Health Community-Based Organized Networks of Equitable Care and Treatment (BH-CONNECT) workforce initiative administered by the Department of Health Care Access and Information (HCAI). Counties must prioritize available BH-CONNECT and other state-administered workforce programs whenever possible.
BHSS funds must be used to:
Supplement workforce activities funded through BH-CONNECT and other state- administered programs (e.g., stipends for childcare or transportation to supplement a retention bonus available through the BH-CONNECT workforce initiative).
Create WET programs within the county that complement state-administered workforce programs.
A.4.2 WET Allowable Activities
WET activities must only address the needs of the county behavioral health delivery system. Activities that may be supported with BHSS funds include, but are not limited to, the following[6]:
Workforce recruitment, development, training, and retention
Professional licensing and/or certification testing and fees
Loan repayment
Retention incentives and stipends
Internship and apprenticeship programs
Continuing education
Efforts to increase the racial, ethnic, and geographic diversity of the behavioral health workforce (e.g., individuals with lived experience)
Staff time spent supervising interns and/or residents who are providing direct county behavioral health services through an internship or residency program.
BHSS funds for WET activities may not be used to:
Address the workforce recruitment and retention needs of systems other than the county behavioral health delivery system, such as criminal justice, social services, and other non-behavioral health systems, although county behavioral health may choose to partner with other systems in order to meet the intersecting needs of its clients.
Pay for staff time spent providing direct behavioral health services.
Employers must not be reimbursed for the time an employee takes from their duties to attend training.
Off-set lost revenues that would have been generated by staff who participate in WET programs and/or activities.
Counties may also use BHSS funds to support administration and coordination of all WET programs and activities (e.g., hiring a WET coordinator).
County-operated and/or county-contracted providers that are employed or volunteer in the county behavioral health delivery system may participate in WET activities. Certain WET activities require a commitment to employment in the county behavioral health delivery system over a certain time. Additional information on WET activities is provided in subsequent sections (Chapter 7, Sections A.4.3 – A.4.9).
A.4.3 Workforce Recruitment, Development, Training, and Retention
Counties may use BHSS funds for county-operated and county-contracted behavioral health workforce recruitment, development, training, and retention activities that include the following:
Recruitment and Retention
Recruitment and retention activities may include, but are not limited to, the following:
Supporting workforce recruitment, including recruiting culturally and linguistically competent staff.
Providing financial incentives to recruit or retain employees.
Providing supported employment services to employees and individuals seeking employment.
Creating and implementing promotional opportunities and policies that promote job retention.
Establishing Regional Partnerships to support recruitment and retention.
Providing wellness activities that promote retention and decrease burnout.
Training and Technical Assistance
Training and technical assistance activities may include, but are not limited to, the following:
Education and training programs and activities for prospective and current employees, contractors, and volunteers.
Collaboration and partnerships to develop curricula and provide training to groups such as individuals receiving services and their family members; individuals from underrepresented racial/ethnic, cultural, and linguistic communities; and other unserved or underserved communities.
Activities that incorporate the input of individuals receiving services and their family members and, whenever possible, utilize them as trainers and consultants in WET programs and/or activities.
Activities that promote cultural and linguistic competence and incorporate the input of diverse racial/ethnic populations that reflect California's general population into WET programs and/or activities.
Payment to trainers for training, technical assistance, and consulting, and travel expenses of trainers and participants, including mileage, lodging, and per diem.
Other costs of providing training, such as materials, supplies, and room and equipment rental costs; also staffing support around administrative tasks, such as paperwork and billing.
Evaluation of the effectiveness of the training and its impact on service delivery.
Employees, contractors and volunteers in non-behavioral health systems, such as criminal justice, social services and health care may participate in training and technical assistance programs and activities; however, they cannot be the sole recipients.
Behavioral Health Career Pathway Programs
Behavioral health career pathway activities may include, but are not limited to, the following:
Programs to prepare individuals receiving services and/or their family members for employment and/or volunteer work.
Programs and coursework in high schools, adult education, regional occupational programs, colleges, and universities that introduce individuals to and prepare them for employment.
Career counseling, training, placement programs, and/or outreach that increase access to employment to unserved and underserved groups and individuals who share the racial/ethnic, cultural, and/or linguistic characteristics of individuals receiving services, their family members, and others in the community with behavioral health needs.
Supervision of employees that are in a Behavioral Health Career Pathway Program.
Workforce Staffing Support
Workforce staffing support may include, but are not limited to, the following activities:
Staff to plan, recruit, coordinate, administer, support, and/or evaluate WET programs and activities when the staff is not funded through any of the other funding components.
Staff to support Regional Partnerships[7] when performing activities that address the following:
Shortages within the workforce or shortages of workforce skills identified as critical by the Regional Partnership.
Deficits in cultural and/or linguistic competence.
Promotion of employment and career opportunities for individuals receiving services and their family members.
Staff to provide ongoing employment and educational counseling and support to individuals receiving services and/or their family members who are entering or currently employed in the workforce.
Staff to provide education and support to employers and employees to assist with the integration of individuals receiving services and/or their family members into the workforce.
A.4.4 Professional Licensing and/or Certification Testing and Fees
Counties may use BHSS funds to cover fees associated with preparing for, applying for, or renewing a license or certification for individuals who are employed, on a full- or part-time basis, in the county behavioral health delivery system.
Counties may support a wide range of activities related to licensing and certification including, but not limited to:
Any fees associated with preparing for, applying for, or renewing a license or certification, such as:
Academic membership fees
Application fees, including fees to obtain academic transcripts or have photos taken of the applicant
Exam fees
Background check fees
License renewal fees
Board of Behavioral Sciences (BBS) registration fees
Fees associated with transferring a license or certification from another state to California
Transportation fees associated with preparing for, applying for, or renewing a license or certification
Any activities that enable provider testing for a license or certification, such as training courses, costs of study material, or coaching.
A.4.5 Loan Repayment
Counties may use BHSS funds to establish locally administered loan repayment programs that pay a portion of the educational loans of individuals who make a commitment to work in the county behavioral health delivery system. Counties have the flexibility to establish loan repayment programs that meet local needs but must adhere to the following minimum requirements.
Eligible Educational Loans
Only loans held by an educational lending institution are eligible for assumption. Eligible educational loan programs include but are not limited to:
The Federal Family Education Loan Program in 20 U.S.C. Sec. 1071 et seq.
The Federal Direct Loan Program in 20 U.S.C. Sec. 1087b et seq.
The following fiscal liabilities are not eligible for loan assumption:
An educational loan(s) that has not been disbursed at the time the applicant signs a loan assumption application and a loan assumption agreement
An educational loan that was used for the educational expenses of someone other than the applicant
An educational loan that has been consolidated with a loan of another person or with a non-educational loan
Lines of credit
Home equity loans
Credit card debt
Business loans
Mortgages
Personal loans
Other consumer loans
Eligible Participants and Service Providers
Individuals must be employed on a full- or part-time basis and must commit to a county-determined term of employment. Counties must ensure terms of employment are met and establish processes to recoup funds should recipients not meet their service commitments, when appropriate.
Maximum Repayment Amount
Loan repayment will be subject to the maximum repayment amounts in alignment with the BH-CONNECT workforce initiative:
There is no lifetime limit on loan repayment amount.
Up to $240,000 per licensed practitioner with prescribing privileges and individuals in training to be a licensed practitioner with prescribing privileges, including but not limited to: Psychiatrists, Addiction Medicine Physicians, and Psychiatric Mental Health Nurse Practitioners.
Up to $180,000 per non-prescribing licensed or associate level pre-licensure practitioner, including but not limited to: Psychologists, Clinical Social Workers, Professional Clinical Counselors, Marriage and Family Therapists; Occupational Therapists, and Psychiatric Technicians
Up to $120,000 per Alcohol or Other Drug Counselors, Community Health Workers, Peer Support Specialists, Wellness Coaches, and other non-prescribing practitioners meeting the provider qualifications for Community Health Worker services, Rehabilitative Mental Health Services, Substance Use Disorder Treatment Services, and Expanded Substance Use Disorder Treatment Services in the California Medicaid State Plan.
Service Obligation
Counties have the flexibility to define service obligations for participants that are commensurate with the loan repayment amount for up to two years for each year of loan repayment. Counties must ensure service obligations are met and have processes to recoup funds if commitments are not met.
Payments
Payments must be made directly to the lending institution and must be applied to the principal balance, if not otherwise prohibited by law or by the terms of the loan agreement between the participant and the educational lending institution.
A.4.6 Retention Incentives and Stipends
Retention incentives and stipends pay or reimburse individuals directly for expenses, or a portion of the expenses, associated with employment or participation in training, educational programs, or other activities in preparation for working in the county behavioral health delivery system. Employment must be on a full- or part-time basis, and recipients must commit to a county-determined term of employment that is commensurate with the incentive or stipend amount. Counties must ensure that the terms of employment are met and must establish processes to recoup funds should recipients not meet their service commitments.
The county may contract with a fiduciary entity, university, or accredited educational institution to establish incentive and stipend programs.
Counties have the flexibility to define which expenses are eligible for retention incentives and stipends and the level of payment. Examples of these types of incentives and stipends include:
Scholarships, which may include, but are not limited to:
Tuition
Registration fees
Books and supplies
Room and board
Childcare
Eldercare
Transportation
Other costs and fees associated with attending an educational program
Recruitment bonuses and retention bonuses, which may include, but are not limited to:
Signing bonuses
Performance bonuses
Spot bonuses
Referral bonuses
Retention incentives and stipends, which may include, but are not limited to:
Travel expenses including commuting to work and mileage, lodging and per diem if travel is for the purpose of participating in an educational or training activity or for professional travel
Home office costs
Professional insurance
Childcare
Eldercare
Wellness
Moving or relocation expenses
Housing
Cellphone or internet services to support employment
Training and professional development costs
As described above, county BHSS funds should supplement activities funded through the BH-CONNECT or other state-administered workforce initiative. Use of BHSS funds to supplement BH-CONNECT programs may be particularly beneficial in scenarios where certain costs are not allowable as part of the BH-CONNECT workforce program. For example, counties may use BHSS funds for stipends for childcare, housing, or other wraparound supports as an “add-on” to a recruitment or retention bonus available through BH-CONNECT.
A.4.7 Internship and Apprenticeship Programs
Counties may use BHSS funds for internship and apprenticeship programs. For activities that involve supervision of post-graduate interns, only faculty time spent supervising interns in programs designed to lead to licensure or certification may be funded.
Activities and expenses that may be funded as part of residency and internship programs include but are not limited to:
Time required of staff, including university faculty, to supervise psychiatric residents or post-graduate interns training to work as psychiatric nurse practitioners; masters of social work; marriage and family therapists; clinical psychologists; clinical counselors; licensed marriage and family therapists; or certified addiction treatment, substance use disorder, or alcohol and other drug counselors.
Time required of staff, including university faculty, to train psychiatric technicians or to train physician assistants to work in the county behavioral health delivery system and to prescribe psychotropic medications under the supervision of a physician.
Addition of a mental health specialty to a physician assistant program.
A.4.8 Continuing Education
Counties may support a wide range of activities related to continuing education in order to develop and retain a well-trained behavioral health workforce, including:
Costs associated with both virtual and in-person continuing education opportunities, including:
Registration fees.
Development and preparation for continuing education, including expenses and consulting fees.
Payment to trainers.
Other costs of providing continuing education, such as materials, supplies, and room and equipment rental costs.
Travel expenses of trainers and county behavioral health delivery system participants, including mileage, lodging and per diem.
Costs associated with purchasing or renewing online training systems or platforms that offer continuing education courses.
A.4.9 Efforts to Increase the Racial, Ethnic, and Geographic Diversity of the Behavioral Health Workforce
Counties may use BHSS funds for activities to increase the racial, ethnic, and geographic diversity of the behavioral health workforce, including incorporating individuals with lived experience into the workforce. Efforts to diversify the workforce should be incorporated across WET activities in recognition of the need to develop a culturally and linguistically competent workforce that can meet the behavioral health needs of individuals of all backgrounds.
A.5 Capital Facilities and Technological Needs
Counties may use a portion of BHSS funds for Capital Facilities and Technological Needs (CFTN). BHSS CFTN projects include the acquisition and development of land, the construction or renovation of buildings, or the development, maintenance, or improvement of information technology to support behavioral health administration and services. Counties can also use BHSS funds as the required match for Behavioral Health Infrastructure Bond Act of 2023 Behavioral Health Continuum Infrastructure Program (BHCIP) awards. BHSS funds for CFTN projects must be spent within ten years, after which unspent funds will be subject to reversion. All transfers into CFTN are irrevocable and cannot be transferred out of CFTN. Additional information on fiscal policies can be found in Chapter 6, Sections B.7 and B.8.
A.5.1 Capital Facilities
BHSS funds may be used by counties for capital facility expenditures. Funds may be used to acquire, develop, or renovate buildings or to purchase land in anticipation of acquiring/constructing a building. Capital facility activities do not include Housing Interventions.
Capital facilities funds must be used for land and buildings, including administrative offices, that support behavioral health administration and services and enable the county to meet objectives outlined in its Integrated Plan. BHSS funds may be used by counties for capital facility expenditures for county owned and county contracted providers providing behavioral health services to the county. Specific allowable uses include:
Acquiring and building upon land that will be county-owned.
Acquiring, constructing, or renovating buildings that are or will be county-owned (e.g., residential care/treatment facilities, clinics, clubhouses, wellness and recovery centers, office spaces, or buildings where behavioral health vocational, educational, and recreational services are provided). The building can be owned and operated by a non-profit if the non-profit is providing behavioral health services under contract with the county.
Establishing a capitalized repair/replacement reserve for buildings, including administrative offices, that enable the county to meet objectives outlined in its Integrated Plan and/or personnel costs directly associated with a capital facilities project.
Renovating buildings that are county or privately owned if the building is dedicated and used to provide county behavioral health services.
Acquiring facilities not secured to a foundation that is permanently affixed to the ground (e.g., vehicles that provide mobile medication for opioid use disorder services, modular buildings for behavioral health services located on school grounds). Acquisition of these facility types is permissible for both the county and for non-profit behavioral health providers.
Meeting the match requirements for Behavioral Health Infrastructure Bond Act of 2023 BHCIP awards (Bond BHCIP). Capital facilities funds used as a match for Bond BHCIP awards must meet all Bond BHCIP requirements. The use of BHSA funds for BHCIP match requirements is permissible for both the county and for non-profit behavioral health providers.
The following additional requirements apply to capital facilities projects:
BHSS funds for capital facilities can only be used for those portions of land and buildings where county behavioral health services are provided.
Land acquired and built upon or construction/renovation of buildings using BHSS funds must be used to provide county behavioral health services for a minimum of twenty years.
All buildings under this component must comply with federal, state, and local laws and regulations, including zoning and building codes and requirements; licensing requirements, where applicable; fire safety requirements; environmental reporting and requirements; hazardous materials requirements; the Americans with Disabilities Act (ADA), California Government Code Section 11135, and other applicable requirements.
Capitalized repair/replacement reserves must be controlled, managed, and disbursed by the county.
Counties may “lease (rent) to own” a building if “lease (rent) to own” is preferable to the outright purchase of the building and the purchase of such property, with BHSS funds, is not feasible. Counties must provide information on why the purchase of the property is not feasible in their Integrated Plan.
County Behavioral Health Departments may purchase land with BHSS funds even if they do not plan to use BHSS funds for the construction of a building or purchase of a building (e.g. modular, etc.) if they have other expected sources of income for the planned construction or purchase of a building upon this land and the purchase serves to increase the county’s infrastructure. The purchase must serve to increase the county’s infrastructure for behavioral health services. Counties must include an explanation of the timeline and expected sources of income for the land in their Integrated Plan.
Examples of costs for which BHSS funds may not be used for capital facilities activities include:
Facilities where the purpose of the building is to provide housing.
Master leasing or renting of building space.
Purchase of vacant land with no plan for building construction.
Acquisition of land and/or buildings and/or construction of buildings, and establishment of a capitalized repair/replacement reserve when the owner of record is a nongovernment entity.
Operating costs for the building (e.g., insurance, security guard, taxes, utilities, landscape maintenance, etc.).
Furniture or fixtures not attached to the building (e.g., desks, chairs, tables, sofas, lamps, etc.).
A.5.2 Technological Needs
BHSS funds may be used to 1) increase individual and family empowerment and engagement by providing the tools for secure access to their health information and 2) modernize and transform clinical and administrative information systems. Counties may combine their resources to advance multi-county technological needs projects.
BHSS funds may be used for technological needs expenditures that support behavioral health administration and services including, but not limited to, the following:
Electronic health record (EHR) system projects including but not limited to:
Infrastructure, security, privacy
Practice management
Clinical data management
Computerized provider order entry
Full EHR with interoperability components (for example, standard data exchanges with other counties, contract providers, labs, pharmacies)
Individual and family empowerment projects including but not limited to:
Individual/family access to computing resources projects
Personal health record system projects
Online information resource projects (expansion/leveraging information sharing services)
Other technological needs projects and expenditures that support behavioral health operations including but not limited to:
Telemedicine and other rural/underserved service access methods
Pilot projects to monitor new programs and service outcome improvement
Data warehousing projects/decision support
Imaging/paper conversion projects
Multi-county technological needs projects
Maintenance costs, such as subscriptions to maintain EHRs or other systems
Resources to support compliance with the Americans with Disabilities Act (ADA) Title II requirements for web content and mobile app accessibility, California Government Code Section 11135 and other applicable requirements.
A.6 Innovative Behavioral Health Pilots and Projects
The goal of innovative behavioral health pilots and projects is to build the evidence base for the effectiveness of new statewide strategies. Counties are encouraged to pilot and test innovative behavioral health pilots and projects in all BHSA funding components (Housing Interventions, FSP, and BHSS).[8] Counties should fund innovative behavioral health pilots and projects under each of those separate funding components.
A.7 Early Intervention Programs
Under the Mental Health Services Act, Prevention and Early Intervention made up one of the five program components. Now, Early Intervention is covered under BHSS to be provided by counties and four percent of total BHSA funding will be used by the California Department of Public Health (CDPH) for statewide Population-Based Prevention programs and activities.
Under BHSA, each county must establish and administer an Early Intervention program that is designed to prevent mental illnesses and substance use disorders from becoming severe and disabling and to reduce disparities in behavioral health.[9] At least 51 percent of BHSS funding must be used to fund Early Intervention programs and services. At least 51 percent of the BHSS Early Intervention funding must be used to serve eligible individuals who are 25 years of age and younger, including transitional aged youth.[10] Early Intervention funds may also be used to provide supports and services to parents and caregivers. However, these services do not count toward the 51% requirement spent on individuals who are 25 years and younger. Early Intervention funds can also be used to support innovative behavioral health pilots and projects within these parameters to build the evidence base for the effectiveness of new statewide strategies.[11]
County Early Intervention programs must also include a Coordinated Specialty Care for First Episode Psychosis (CSC for FEP) program beginning July 2026. More information on CSC-FEP requirements can be found in Chapter 7, Section A.7.5.
County Early Intervention programs must emphasize the reduction of the likelihood of the following adverse outcomes for BHSA eligible individuals:[12]
Suicide and self-harm
Incarcerations
School suspension, expulsion, referral to an alternative or community school, or failure to complete (inclusive of early childhood zero to five years of age, Transitional Kindergarten (TK)-12, and higher education)
Unemployment
Prolonged suffering
Homelessness
Removal of children from their homes
Overdose
Mental illness in children and youth through social, emotional, developmental, and behavioral services and supports in early childhood
Culturally Responsive and Linguistically Appropriate Interventions
County Early Intervention programs must include culturally responsive and linguistically appropriate interventions. These interventions must be able to reach underserved cultural populations[13] and address specific barriers related to racial, ethnic, cultural, language, gender, sexual orientation, gender identity, religion, age, economic, or other disparities in mental health and substance use disorder treatment services access, quality, and outcomes.[14]
County Early Intervention programs must create critical linkages with community-based organizations, including, but not limited to, service and treatment providers, youth centers, licensed and exempt clinics, facilities and providers licensed or certified by the DHCS, licensed or certified residential substance use disorder facilities, and licensed narcotic treatment programs. Community-based organizations may also include organizations that provide evidence-based practices (EBPs) or community-defined evidence practices (CDEPs).[15]
Counties are encouraged to partner with community-based organizations that specialize in serving specific populations that are underserved and address specific barriers in the above paragraphs. DHCS encourages the use of CDEPs at the local level to address historical behavioral health disparities. CDEPs are an alternative or complement to EBPs, that offer culturally anchored interventions that reflect the values, histories and life experiences of the communities that the provider is providing services. These practices come from the community and the organizations that serve them and are found to yield positive results as determined by community consensus over time.
A.7.1 Early Intervention
Early Intervention is the proactive approach of identifying and addressing behavioral health concerns in their early stages before they escalate into more severe, disabling or chronic conditions. DHCS has adapted the Institute of Medicine’s Continuum of Care to clarify the types of behavioral health services and supports that can be funded under BHSS Early Intervention programs.[16]
Under the Institute of Medicine’s Continuum of Care model, there is a spectrum that spans prevention and early intervention, and within the spectrum, there are differentiations based on type of intervention.
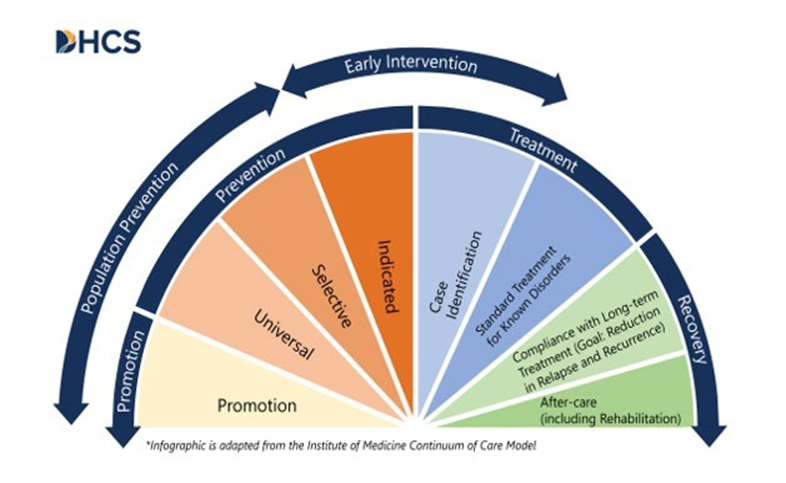
Figure 7.A.1. The Institute of Medicine’s Continuum of Care and Spectrum of Early Intervention Services
Under this model, Early Intervention must focus on strategies and activities that are directed to an eligible individual, including indicated prevention and case identification.
Early Intervention services may be provided to individuals lacking a specific diagnosis. Indicated prevention interventions focus on BHSA eligible at-risk individuals who are at risk or and experiencing early signs of a mental health or substance use disorder or who have experienced known risk factors for poor behavioral health outcomes, such as trauma, Adverse Childhood Experiences, or involvement with child welfare or corrections system. This at-risk individual may not yet meet the criteria of a diagnosable mental health or substance use disorder. Indicated prevention is the only prevention intervention that is allowable under Early Intervention, as shown in Figure 7.A.1. Examples of indicated interventions include, but are not limited to, outreach, training, and education for high-risk individuals and/or families who are at risk and experiencing early signs of a mental health or substance use disorder. Indicated interventions are preventive and often provided before an individual receives or meets diagnostic criteria for a behavioral health diagnosis. Case identification includes assessment, diagnoses, brief interventions, and activities needed to create access and linkages to care that connect individuals to the appropriate care.
County Early Intervention programs target BHSA priority populations and have the goal of identifying these individuals for access and linkage to services and treatment as needed. Additional information on BHSA eligible and priority populations can be found in Chapter 2, Section B.3.
A.7.2 Priorities for Use of Funds
County Early Intervention programs must focus on the following priorities[17]:
Childhood trauma early intervention to deal with the early origins of mental health and substance use disorder treatment needs, including strategies focused on:
Eligible children and youth experiencing homelessness.
Justice-involved children and youth.
Child welfare-involved children and youth with a history of trauma.
Other populations at risk of developing a mental health disorder or condition as specified in subdivision (d) of WIC 14184.402 or substance use disorders.
Eligible children and youth in populations with identified disparities in behavioral health.[18]
Early psychosis and mood disorder detection and intervention and mood disorder programming that occurs across the lifespan.
Outreach and engagement strategies that target early childhood zero to five, out-of-school youth, and secondary school youth. Partnerships with community-based organizations and college mental health and substance use disorder programs may be used to implement the strategies.
Culturally responsive and linguistically appropriate interventions.
Strategies targeting the mental health and substance use disorder needs of older adults.
Strategies targeting the mental health needs of eligible children and youth, as defined in W&I Code section 5892, who are zero to five years of age, including, but not limited to, infant and early childhood mental health consultation.
Strategies to advance equity and reduce disparities.
Strategies to address the needs of individuals at high risk of crisis.
Programs that include community-defined evidence practices and evidence-based practices and mental health and substance use disorder treatment services similar to those provided under other programs that are effective in preventing mental illness and substance use disorders from becoming severe and components similar to programs that have been successful in reducing the duration of untreated severe mental illness and substance use disorders to assist people in quickly regaining productive lives.
While the above priorities are required, counties may include other priorities for the use of their BHSS Early Intervention funds based on needs identified in their community planning process, in addition to the established priorities and consistent with Chapter 3, Section B.[19] If a county chooses to include other programs, the Integrated Plan shall include a description of why those programs are included and metrics by which effectiveness of those programs is to be measured.[20] Counties may act jointly to meet these requirements.[21]
A.7.2.1 Childhood Trauma Early Intervention Programs[22]
The BHSA strengthens prioritization of resources to serve eligible children and youth with its dedicated allocation of BHSS Early Intervention funds. County Early Intervention programs must include specific interventions focused on childhood trauma.
These programs target BHSA eligible children and youth exposed to, or who are at risk of exposure to, adverse childhood experiences (ACEs) and traumatic childhood events, environmental trauma including community violence, generational trauma, institutional trauma, and prolonged toxic stress. Childhood trauma Early Intervention programs aim to address the early origins of mental health and substance use disorder needs and prevent long-term mental health and substance use disorder concerns. These programs may include, but are not limited to, the following:
Focused outreach and early intervention to at-risk and in-need populations, including youth experiencing homelessness, justice-involved youth, LGBTQ+ youth, and child welfare-involved youth.
Implementation of appropriate trauma and developmental screening and assessment tools with linkages to early intervention services to eligible children and youth who qualify for these services.
Collaborative, strengths-based approaches that appreciate the resilience of trauma survivors and support their parents and caregivers when appropriate.
Support from peer support specialists, wellness coaches, and community health workers trained to provide mental health and substance use disorder treatment services with an emphasis on culturally and linguistically tailored approaches.
Multigenerational family engagement, education, and support for navigation and service referrals across systems that aid the healthy development of children and youth and their families.
Collaboration with county child welfare agencies and other system partners, including Medi-Cal Managed Care Plans, and homeless youth service providers, to address the physical and behavioral health-related needs and social needs of child-welfare-involved youth.
Linkages to primary care and behavioral health settings, including, but not limited to, federally qualified health centers, rural health centers, community-based providers, school-based health centers, school-linked providers, and school- based programs and community-based organizations, early learning and care centers, Regional Centers, school-based health centers, specializing in serving underserved communities.
Linkages to county and community-based organizations that will help address the adolescent’s needs through the provision of continuing care and support services.
Leveraging the healing value of traditional cultural connections and faith-based organizations, including policies, protocols, and processes that are responsive to the racial, ethnic, and cultural needs of individuals served and recognition of historical trauma.
Blended funding streams to provide individuals and families experiencing toxic stress comprehensive and integrated supports across systems.
Partnerships with local educational agencies and school-based behavioral health professionals, early learning and care centers, county First Five commissions, and Regional Centers, to identify and address children exposed to, or who are at risk of exposure to, adverse and traumatic childhood events and prolonged toxic stress.
A.7.3 Early Intervention Program Components
Each county must establish and administer an Early Intervention program that is designed to prevent mental illnesses and substance use disorders from becoming severe and disabling and to reduce disparities in behavioral health. County Early Intervention programs must include the following components[23]:
Outreach
Access and linkage to care
Mental health and substance use disorder early treatment services and supports
All services and supports provided within county Early Intervention programs must meet the requirements of their respective component.
A.7.3.1 Outreach
Outreach is the process of engaging, encouraging, educating, training, and learning about ways to recognize and respond effectively to early signs of potentially severe and disabling mental health and substance use disorders.[24] Outreach activities funded under BHSS Early Intervention must meet the following requirements:
Be directed towards eligible high-risk individuals within BHSA priority populations,[25] including older adults[26] and youth.[27]
Have the goal of identifying individuals for access and linkage to services and supports.
Connect eligible individuals directly to access and linkage programs or to mental health and substance use disorder treatment services and supports, should an individual wish to be connected to services.
County outreach activities may include those that target:
Families
Employers
Primary care health care providers
Behavioral health urgent care and first responders
Hospitals, inclusive of emergency departments
Education, including early care and learning, TK-12, higher education
Community-based organizations that specialize in serving underserved communities
Others
Eligible older adults and youth may require tailored outreach strategies, as noted below.
Outreach Strategies for Older Adults
When targeting the mental health and substance use disorder needs of BHSA eligible older adults, outreach strategies include, but are not limited to, the following[28]:
Outreach and engagement strategies that target caregivers, victims of elder abuse, and individuals who live alone.
Outreach to older adults who are isolated and/or lonely.
Programs for early identification of mental health disorders and substance use disorders.
Outreach to organizations that provide services to older adults such as Area Agencies on Aging, Caregiver Resource Centers, and Aging and Disability Resource Connections.
Youth Outreach and Engagement
Youth outreach and engagement strategies target BHSA eligible out-of-school youth and secondary school-age youth, and include, but are not limited to, the following[29]:
Establishing direct linkages for youth to community-based mental health and substance use disorder treatment services.
Participating in EBPs and CDEP programs for mental health and substance use disorder treatment services.
Providing supports to facilitate access to services and programs, including those utilizing EBPs and CDEPs, for underserved and vulnerable populations, including, but not limited to, members of ethnically and racially diverse communities, members of the LGBTQ+ communities, victims of domestic violence and sexual abuse, and veterans.
Establishing direct linkages for students to community-based behavioral health services for which reimbursement is available through the students’ health coverage.
Reducing racial disparities in access to behavioral health services.
Providing school employees and students with education and training in early identification, intervention, and referral of students with behavioral health needs.
Providing education and training opportunities in early identification, intervention, and referral of youth with behavioral health needs in community- based settings to target out-of-school youth and employees of organizations that work with youth.
Providing strategies and programs for youth with signs of behavioral or emotional needs or substance misuse who have had, or are at risk of having, contact with the child welfare or juvenile justice system.
Providing integrated youth behavioral health programming.
A.7.3.2 Access and Linkage to Care
Access and linkage to care must ensure that care can be provided by county behavioral health programs as early in the onset of behavioral health conditions as practicable, and that referrals for medical and social services are provided as needed.[30] Access and linkage to care may include activities that support screening, assessment, and referral to behavioral health services, such as telephone help lines, mobile response teams, and supportive services such as Enhanced Care Management and Community Supports available to Medi-Cal members. Activities must also include the scaling of and referral to the Early Psychosis Intervention (EPI) Plus Program, including Coordinated Specialty Care, or other EBPs and CDEPs for early psychosis and mood disorder detection and intervention programs.[31]
A.7.3.3 Mental Health and Substance Use Disorder Services and Supports
Mental health and substance use disorder treatment services and supports provided under Early Intervention must be proven to reduce the duration of untreated serious mental health illnesses and substance use disorders and assist people in quickly regaining productive lives.[32],[33] Early intervention mental health and substance use disorder services must also be responsive to the cultural and linguistic needs of diverse communities.[34]
When determining what practices to implement locally, counties may reference the biennial DHCS-provided list of EBPs and CDEPs.[35] More information on EBPs and CDEPs can be found in Chapter 7, Section A.7.6.
Early intervention mental health and substance use disorder treatment services and supports to those eligible for BHSA may include:
Mental health treatment services to address first episode psychosis.
Mental health and substance use disorder services that prevent, respond, or treat a behavioral health crisis or activities that decrease the impacts of suicide, return to use of illicit substances or misuse of prescription drugs, and/or accidental overdose/poisoning.
Early intervention services designed to address co-occurring mental health and substance use issues.
In addition to the BHSA Eligible Populations, early intervention mental health and substance use disorder services may be provided to the following eligible children and youth.
Individual children and youth at high risk for a behavioral health disorder due to experiencing trauma, as evidenced by scoring in the high-risk range under a trauma screening tool such as an ACEs screening tool,[36] involvement in the child welfare system or juvenile justice system or experiencing homelessness.
Individual children and youth in populations with identified disparities in behavioral health outcomes.
A.7.4 Stigma and Discrimination Reduction
Stigma and discrimination reduction activities aim to reduce negative feelings, attitudes, beliefs, perceptions, stereotypes, and/or discrimination related to being diagnosed with a mental illness, substance use disorder or seeking behavioral health services. Stigma and discrimination reduction programs align with population-based prevention activities and cannot be funded with Early Intervention funding.
A.7.5 Early Psychosis Intervention Plus Programs[37]
Early Psychosis Intervention (EPI) Plus programs encompass early psychosis and mood disorder detection and intervention. These programs utilize evidence-based approaches and services to identify and support clinical and functional recovery of individuals by reducing the severity of first, or early, episode psychotic symptoms and other early markers of serious mental illness, such as schizophrenia spectrum disorders and mood disorders, supporting individuals to engage in school or at work, and putting them on a path to better health and wellness.[38] EPI Plus programs may include, but are not limited to, all of the following:
Focused outreach to at-risk and in-need populations, as applicable.
Recovery-oriented psychotherapy, including cognitive behavioral therapy focusing on co-occurring disorders.
Family psychoeducation and support.
Peer support services.
Supported education and employment.
Pharmacotherapy and primary care coordination.
Use of innovative technology for mental health information feedback access that can provide a valued and unique opportunity to assist individuals with mental health needs and to optimize care.
Case management.
EPI Plus programs must include CSC for FEP and may include other EBPs and CDEPs for early psychosis and mood disorder detection and intervention programs. See CSC for FEP requirements below.
A.7.5.1 Coordinated Specialty Care for First Episode Psychosis
CSC for FEP is a community-based service that provides timely and integrated support during the critical initial stages of psychosis with the strongest base of evidence among any intervention for improving outcomes for individuals experiencing early psychosis. CSC for FEP reduces the likelihood of psychiatric hospitalization, emergency room visits, residential treatment placements, involvement with the criminal justice system, substance use, and homelessness that are often associated with untreated psychosis.[39],[40] Research on CSC for FEP has demonstrated that individuals who receive this service are significantly less likely to develop a significant mental health condition over time compared to those who receive standard care.[41] Individuals who receive CSC for FEP have also reported improved psychopathology and overall quality of life.[42] DHCS and the Mental Health Services Oversight and Accountability Commission (MHSOAC) have made significant investments in expanding CSC for FEP throughout the state, such as through funding, technical assistance, and policy reforms. These efforts include contracting with University of California, Davis to fund FEP technical assistance for county behavioral health agencies, a $25 million commitment to further support and expand EPI-CAL, Assembly Bill (AB) 1315 establishment of the EPI Plus program, Children and Youth Behavioral Health Initiative (CYBHI) grants for CSC for FEP, and coverage of CSC for FEP as a bundled service under Behavioral Health Community-Based Organized Networks of Equitable Care and Treatment (BH-CONNECT).
County Early Intervention programs must implement CSC for FEP beginning July 2026. In addition to utilizing EI funds under BHSS, counties may meet the requirement to implement CSC for FEP programs using other non-BHSA funding sources including, but not limited to 2011 Realignment or Mental Health Block Grant funding, so long as this is accounted for in their Integrated Plan. To support implementation, DHCS will make available training, technical assistance, and fidelity monitoring supports for counties as they implement CSC for FEP.
Between July 1, 2026, and June 30, 2029, all counties[43] must:
Participate in ongoing training and technical assistance.
Understand gaps to fidelity by December 31, 2027.
Complete full fidelity reviews and demonstrate counties are implementing CSC for FEP with fidelity by June 30, 2029.
A.7.5.2 Aligning Coordinated Specialty Care for First Episode Psychosis in Early Intervention with Medi-Cal
In December 2024, CMS approved State Plan Amendment (SPA) 24-0042, which establishes CSC for FEP as a covered benefit in the Medi-Cal program. Counties have the option to provide CSC for FEP as a bundled service with a monthly bundled reimbursement rate under Medi-Cal in the Specialty Mental Health Services (SMHS) delivery system beginning in 2025.[44]
Counties should use the BH-CONNECT EBP Policy Guide to support implementation of CSC for FEP. The EBP Policy guide includes information about the evidence-based service criteria for CSC for FEP, staffing structure for teams of behavioral health practitioners delivering CSC for FEP, and other best practices for delivering CSC for FEP with fidelity to the evidence-based model.
In addition, all counties must adhere to the training, technical assistance and fidelity requirements identified in the forthcoming BH-CONNECT EBP Behavioral Health Information Notice (BHIN). The BH-CONNECT EBP BHIN also includes coverage, payment and other compliance requirements for counties that elect to cover CSC for FEP in Medi-Cal.
Counties that do not choose to offer CSC for FEP as a bundled Medi-Cal service are still required to deliver and bill Medi-Cal for medically necessary unbundled CSC for FEP services covered as SMHS.
These services may include the following SMHS:
Assessment
Crisis Intervention
Medication Support Services
Peer Support Services
Psychosocial Rehabilitation
Referral and Linkages
Therapy
Treatment Planning
Even if counties do not opt to take up the option to provide CSC for FEP as a bundled Medi-Cal service, counties must deliver CSC for FEP with fidelity and consistent with the requirements established for BH-CONNECT. For non-Medi-Cal BHSA eligible individuals, Early Intervention funding may be used for the fully uninsured. Commercial health plans are required to provide coverage for CSC for FEP under Senate Bill (SB) 855 regulations[45] and counties are required to seek reimbursement from commercial payers; see section C.3.3 regarding how to file a complaint with the appropriate regulatory agency.[46]
A.7.6 Biennial List of Evidence-based Practices and Community- Defined Best Practices
DHCS will develop a non-exhaustive list of Early EBPs and CDEPs biennially.[47] The biennial list is an optional reference tool to support each county behavioral health department’s community planning process discussions regarding which practices to implement locally.
The only EBP that counties are required to provide as a part of Early Intervention is a CSC for FEP program, beginning July 2026. However, DHCS may require a county to implement a particular EBP or CDEP from the DHCS biennial list.[48]
Counties can include other county-specific CDEPs and can innovate and implement emerging and promising practices that are not included on the biennial list of EBPs and CDEPs provided by DHCS in their IP.
An Early Intervention EBP or CDEP on the biennial list may include population-based prevention elements. Counties will still be able to fund EBPs and CDEPs that may have very limited population-based prevention components in full with BHSS funds only if the EBP or CDEP is on the biennial list developed by DHCS.
DHCS leverages the following sources to identify EBPs and CDEPs:
BH-CONNECT[49]
Children and Youth Behavioral Health Initiative’s (CYBHI) EBPs and CDEPs grant program[50]
Family First Prevention Services Act[51]
Blueprints for Healthy Youth Programs[52]
The Athena Forum created by Washington State Health Care Authority[53]
CDPH’s California Reducing Disparities Project[54]
Evidence-based Practices Resource Center developed by the Substance Abuse and Mental Health Services Administration[55]
The Cognitive-Behavioral Interventions for Substance Use curriculum designed by the University of Cincinnati[56]
California Evidence-Based Clearinghouse for Child Welfare[57]
The County of Los Angeles Department of Mental Health, Prevention and Early Intervention EBPs, Promising Practices, and CDEPs Resource Guide 2.0. created by the California Institute for Mental Health[58]
B. Full Service Partnership
B.1 Full Service Partnership Funding
Counties are required to use 35 percent of the funds distributed by the State Controller’s Office into their Behavioral Health Services Fund (BHSF) for Full Service Partnership (FSP).
B.2 Introduction and Background
FSP programs provide individualized, team-based care to individuals living with significant behavioral health needs through a “whatever it takes” approach. Participants benefit from a community-based, whole-person approach that is trauma-informed, recovery-focused, age-appropriate, and delivered in partnership with families or an individual’s natural supports.
County FSP programs have been a core Mental Health Services Act (MHSA) investment over the last 20 years and continue to be a key component of California’s behavioral health continuum of care. FSP programs were developed from the early successes of late-90s’ pilot programs “to fund comprehensive and integrated care for persons with high risk for homelessness, justice involvement, and hospitalization.”[59] While evaluations have found that county FSP programs achieve improved outcomes for FSP participants and cost savings, there is variance in county models and limited information available on the effectiveness of county FSP programs and the overall FSP initiative.[60] A 2024 Mental Health Services Oversight and Accountability Commission (MHSOAC) publication identified opportunities to improve FSP programs, many of which are reflected in the Behavioral Health Services Act (BHSA). The recommendations include[61]:
Establish a common set of service requirements.
Develop standardized definitions and eligibility requirements.
Develop a tiered system for FSP care and incorporate step-down planning into programs.
Ensure FSP programs are equipped to serve a diverse population.
Streamline data collection and clarify expectations.
Many policy changes that will be implemented under the BHSA are responsive to these MHSOAC recommendations. Under BHSA, FSP policies will include standardization of key evidence-based practices (EBPs) that must be included as part of county FSP programs across service delivery systems, a tiered model with opportunity for step-down planning, and greater consistency in FSP programs from county to county.
B.3 Full Service Partnership Program Requirements
B.3.1 Eligible and Priority Populations
FSP Eligible Populations include:
Behavioral Health Services Act (BHSA) eligible adults and older adults, who meet the priority population criteria specified in W&I Code section 5892, subdivision (d), and
BHSA eligible children and youth, which includes transitional age youth (TAY).
B.3.2 Baseline Requirements
Given the expansion to include eligible individuals living with substance use disorder (SUD) in the BHSA, county FSP programs must include SUD treatment services where appropriate. County FSP teams must be capable of supporting FSP participants living with co-occurring mental health and substance use disorder conditions by providing integrated behavioral health care as part of the FSP program, inclusive of mental health, SUD and/or co-occurring services, or by closely coordinating the provision of SUD care for FSP participants.
FSP services shall be provided in accordance with demonstrated clinical need and in alignment with the required high intensity service models: Assertive Community Treatment (ACT), Forensic ACT (FACT), FSP Intensive Case Management (ICM), and High Fidelity Wraparound (HFW).[62] Please refer to the respective sections for details regarding required services and expectations for co-occurring capabilities.
County FSP programs must provide ongoing engagement services to FSP participants in order to maintain their continued treatment.[63] These services may include clinical and recovery-oriented services, such as consumer-operated services, peer support services, transportation, and services to support maintaining housing.[64]
County FSP programs must also include outpatient behavioral health services, either clinic or field based, necessary for the ongoing evaluation, and stabilization and recovery of an enrolled individual. Many of these outpatient behavioral health services are incorporated within the high intensity service models (ACT, FACT, FSP ICM, and HFW) county FSP programs are required to utilize.
FSP teams are required to coordinate with an FSP program participant’s primary care provider as appropriate. Ensuring coordination across systems, including primary care, is critical to participant engagement and satisfaction.[65]
B.3.3 Full Service Partnership Continuum
In accordance with W&I Code section 5887, county FSP programs must make the following specified services available:[66]
Mental health services, supportive services, and substance use disorder (SUD) services
Assertive Community Treatment (ACT)
Forensic ACT (FACT)
FSP Intensive Case Management (ICM)[67]
Individual Placement and Support (IPS) model of Supported Employment
High Fidelity Wraparound (HFW)
Assertive field-based initiation for SUD
Outpatient behavioral health services for evaluation and stabilization
Ongoing engagement services
Service Planning[68]
Housing Interventions (funded under the Housing Interventions category)
County FSP programs may additionally include behavioral health services the county determines are beneficial to an eligible individual's treatment, if not already covered by ACT, FACT, FSP ICM, or HFW, in collaboration with the individual and, when appropriate, the individual's family. Additional services that may be offered in addition to or in conjunction with the specified services listed above include but are not limited to:
Primary SUD FSPs
Additional evidence-based practices (EBPs)
Outreach
Other recovery-oriented services, including consumer-operated services and peer support services
Counties may use FSP funding for outreach activities if the activities relate to enrolling individuals living with significant behavioral health needs in an FSP.[69] For example, counties are encouraged to use data systems (e.g., Medi-Cal Connect) to identify individuals who are not actively receiving behavioral health care through the county yet meet clinical criteria for FSP, and conduct targeted outreach to those individuals. For individuals receiving one of the required EBPs, initial outreach and ongoing engagement is embedded in the model. General outreach to individuals living with significant behavioral health needs who are not FSP eligible should be funded under other appropriate funding sources including Behavioral Health Services and Supports (BHSS) and Housing Interventions.
B.3.4 Full Service Partnership Exemptions
Fiscal Year (FY) 2026-2029 Integrated Plan
State law permits counties with a population of less than 200,000 to request an exemption from the FSP requirements in W&I Code section 5887, subdivision (a)(2). For the first Integrated Plan covering fiscal years 2026-2029, all counties, regardless of their size, will be exempt from the EBP fidelity requirements for ACT, FACT, IPS Model of Supported Employment, and HFW. Therefore, counties do not need to request an exemption from FSP EBP requirements in their first Integrated Plan. DHCS will make available training, technical assistance, and fidelity monitoring supports for counties as they implement FSP EBPs: ACT, FACT, IPS and HFW. Counties are still required to begin offering the required EBPs by July 1, 2026.
To meet FSP EBP requirements, between July 1, 2026, and June 30, 2029, all counties must:
Participate in ongoing training and technical assistance for all FSP EBPs.
Understand gaps to fidelity for each FSP EBP by December 31, 2027.
Complete full fidelity reviews and demonstrate counties are implementing all FSP EBPs with fidelity by June 30, 2029.[70]
FY 2029-2032 Integrated Plan
Subject to DHCS approval, for the second Integrated Plan covering fiscal years 2029- 2032, small counties (population less than 200,000) may request an exemption from the ACT and FACT EBP. Small counties may also request an exemption from IPS and HFW[71] EBP fidelity requirements.
The criteria for FSP exemption requests include:
Limited workforce (e.g., providers)
Limited need (e.g., the number of individuals eligible is too small for the county to support the required EBP staffing for fidelity)
Other considerations, subject to evidence requirements and DHCS review
Counties may use the findings from COE fidelity reviews and other data to determine whether they will seek an exemption in fiscal year 2029. Exemption requests must include:
Documentation demonstrating that one or more of the criteria for exemption are met (e.g., workforce or county demographic data, COE informational fidelity review findings).
A description of how counties will work towards improving fidelity scores or for counties that may never meet fidelity requirements, an explanation of why.
B.3.5 Full Service Partnership Co-Occurring Capabilities
The American Society of Addiction Medicine (ASAM) Criteria, Fourth Edition defines co- occurring capable as “Achieving co-occurring capability involves looking at all aspects of program design and functioning to embed integrated policies, procedures, practices, and training in the operations of the program to make it routine for clinicians to successfully delivery integrated care.” FSP participants deserve access to co-occurring care consistent with industry standards. To that end, county FSP programs are required to implement the following:[72]
Connecting individuals to FSP teams, SUD providers, or other clinically necessary services including peer support, as appropriate, after they receive assertive field-based initiation for substance use disorder (SUD) treatment services.
Conducting ASAM screening as part of an integrated assessment upon intake into the FSP, and connecting individuals to SUD providers, as appropriate.
Offering medications for addiction treatment (MAT) services directly to clients or having an effective referral process in place (i.e., established relationship with a MAT provider and transportation to appointments for MAT).[73]
Equipping FSP program staff at all levels of care to provide comprehensive care to individuals living with significant co-occurring behavioral health needs (e.g., motivational interviewing, engagement, and training for prescribers who are not familiar or comfortable with prescribing MAT).
Developing strategies for billing and claiming the appropriate service/delivery system within the context of co-occurring care delivery (e.g., Medi-Cal Specialty Mental Health Services (SMHS) versus Drug Medi-Cal (DMC)/Drug-Medi-Cal Organized Delivery System (DMC-ODS).
For individuals living with SUD only, DHCS will allow but will not require SUD-only FSPs (see additional information in the Substance Use Disorder Primary Full Service Partnership Option section).
B.4 Full Service Partnership Levels of Care
Pursuant to W&I Code section 5887, subdivision (e), county Full Service Partnership (FSP) programs are required to have a standard of care, with levels of care to treat individuals based on acuity. The following subsections outline the requirements for the levels of care as they pertain to adults and to children and youth.
Behavioral Health Services Act (BHSA) Eligible Adults and Older Adults:
For BHSA eligible adults and older adults, two levels of coordinated care must be available depending on individualized need for service intensity. These are ACT, a stand-alone EBP as the highest intensity level, and FSP Intensive Case Management (ICM), which can be a standardized step-down level from ACT, or provided in order to avert the higher ACT level of care (see Figure 7.B.4.1). FSP ICM is for individuals who may not meet ACT eligibility criteria, but still have significant behavioral health needs and can benefit from FSP supports. Individuals stepping down from FSP ICM who no longer meet the threshold for FSP level of need can receive outpatient mental health (MH) and SUD services, funded through Behavioral Health Services and Supports (BHSS).
As described in subsequent sections of this manual, county BHSA FSP programs must implement EBPs in alignment with Medi-Cal guidance (where applicable). Medi-Cal guidance may include eligibility criteria and/or guidelines on clinical indicators of need for an ACT level of care. However, DHCS recognizes the role of the clinician and her/his team in determining an individual’s appropriate level of care, and that movement between tiers may not be linear (i.e., the FSP participant may also need to step back up a level). DHCS will not establish requirements for standardized assessments specific to determining FSP levels of care; this is left to counties and to the clinical judgment and discretion of the treating provider. Under BH-CONNECT, DHCS anticipates issuing guidance for use of one or more Level of Care tools (guidance forthcoming). This guidance may assist counties with identifying individuals who need an FSP level of care but commonly used Level of Care tools do not differentiate between levels of high-intensity, community-based care, such as between ACT and FSP ICM.
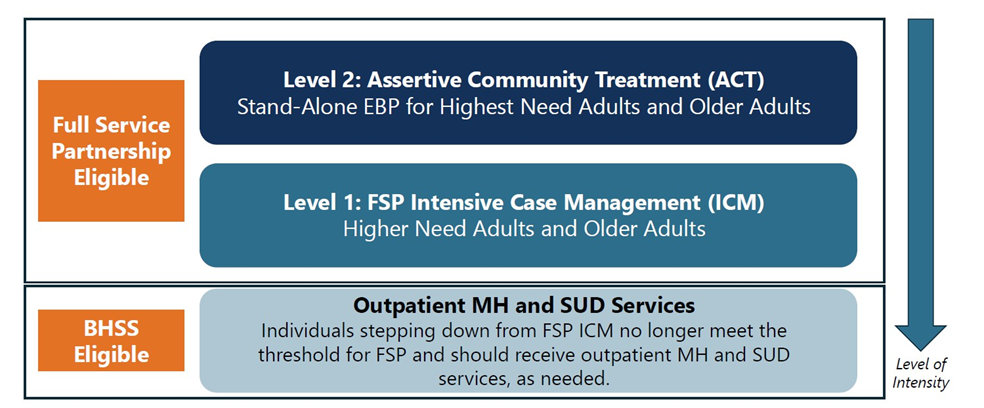
Figure 7.B.4.1. FSP Levels of Care
BHSA Eligible Children and Youth:
For BHSA eligible children and youth, counties shall provide High Fidelity Wraparound (HFW), an especially high intensity, comprehensive, holistic, youth and family-driven way of responding when children or youth experience significant behavioral health challenges. HFW is not restricted to children and youth receiving foster care or involved with child welfare and is intended to support a diverse range of needs and systems interaction.
HFW is the designated FSP level of care for children and youth. However, any child or youth may alternatively receive ACT or FSP ICM, if determined to be clinically and developmentally appropriate.
Among children and youth enrolled in HFW, the array of services required may vary based on individual need. In general, there is little evidence that an additional, lower level of case management – i.e., an approach “beneath” HFW – is effective for children and youth with significant behavioral health needs. As such, DHCS is not currently using its authority under W&I Code section 5887, subdivision (e) to require counties to develop multiple, dedicated levels of case management for FSP for children/youth.
BHSA Eligible Transitional Age Youth (TAY):
BHSA eligible TAY (aged 16-25) and those younger than TAY, may receive ACT, FACT, FSP ICM, or HFW if determined to be clinically and developmentally appropriate by the provider and FSP eligible individual. BHSA eligible TAY are included in the definition for “Eligible children and youth.”[74] Counties shall design FSP programming to meet the needs of all BHSA eligible individuals, including TAY.
Counties must make the appropriate EBP for FSP participants available based on clinical judgment and discretion reflecting individualized needs.
B.4.1 Level 2: Assertive Community Treatment and Forensic Assertive Community Treatment
B.4.1.1 Overview
ACT is an evidence-based practice to support individuals living with complex and significant behavioral health needs and a treatment history that may include psychiatric hospitalization and emergency room visits, residential treatment, involvement with the criminal justice system, homelessness, and/or lack of engagement with traditional outpatient services. ACT is one of the most established and widely researched evidence-based practices in behavioral health care for individuals living with significant mental illness.[75],[76],[77] It has been extensively studied across various populations and settings around the world, with evidence supporting its effectiveness across rural areas, urban centers, and among homeless populations.[78],[79]
Pursuant to the BHSA and as described in the BHSA Fiscal Policies chapter, counties are required to bill Medi-Cal for services when possible instead of using BHSA dollars for the full cost of the service.[80] In alignment with the “whatever it takes” philosophy, FSP funding can be used for services not covered by Medi-Cal, as needed for Medi-Cal members. This includes outreach and engagement services (as outlined in Full Service Partnership Baseline Requirements) and recovery supports, including consumer-operated wellness centers and items that offer emotional support (e.g., a musical instrument).[81] For non-Medi-Cal members, who meet BHSA eligible criteria as defined in W&I code Section 5892, FSP funding may be used for service components that commercial plans do not cover, or for all services for the fully uninsured. For example, pairing an intensive behavioral health service like ACT or FSP Intensive Case Management (ICM) with housing supports is a proven, recommended best practice for achieving long-term housing stability. The FSP component may not be used to fund housing interventions, including for FSP participants. FSP participants may receive housing supports through programs outside the BHSA, or from the BHSA Housing Interventions component, provided that the service is not covered by the participant’s Medi-Cal managed care plan. Pursuant to W&I Code 5830, subdivision (c)(2), BHSA "funds shall not be used for housing interventions covered by a Medi-Cal managed care plan."
FACT builds upon the ACT model to address the complex needs of individuals with significant behavioral health needs who are also involved with the criminal justice system. Individuals with significant and complex behavioral health needs are often overrepresented in jails and prisons, are at higher risk of recidivism upon release, and face barriers to community reintegration, including difficulties accessing treatment, employment, housing, and other supports.
While some counties have historically delivered ACT or services that come close to the full ACT service model as part of their FSP programs, pursuant to BHSA, counties must implement ACT beginning in July 2026.[82]
B.4.1.2 Aligning Assertive Community Treatment and Forensic Assertive Community Treatment in Full Service Partnership with Medi-Cal
In December 2024, Centers for Medicare & Medicaid Services (CMS) approved State Plan Amendment (SPA) 24-0042, which establishes ACT as a covered benefit in the Medi-Cal program, and also provides coverage for FACT. Counties have the option to provide ACT and FACT as bundled services with monthly bundled reimbursement rates in the Medi-Cal SMHS delivery system beginning in 2025.[83]
Counties should use the BH-CONNECT EBP Policy Guide to support implementation of ACT and FACT. The EBP Policy guide includes information about the evidence-based service criteria for ACT and FACT, staffing structure for teams of behavioral health practitioners delivering ACT and FACT, and other best practices for delivering ACT and FACT with fidelity to the evidence-based model.
In addition, all counties must adhere to the training, technical assistance and fidelity requirements identified in the forthcoming BH-CONNECT EBP BHIN. The BH-CONNECT EBP BHIN also includes coverage, payment and other compliance requirements for counties that elect to cover ACT and FACT in Medi-Cal.
Counties that do not choose to offer ACT or FACT as bundled Medi-Cal services are still required to cover and bill Medi-Cal on an unbundled basis for many SMHS that are part of ACT and FACT, including:
Assessment
Crisis intervention
Medication support services
Peer support services
Psychosocial rehabilitation
Referral and linkages
Therapy
Treatment planning
Notably, counties that do not choose to offer ACT or FACT as bundled Medi-Cal services are unable to bill Medi-Cal for key components of ACT and FACT, including employment and education supports as defined in the Medi-Cal state plan, and support for non-billable activities essential to the coordinated, team-based model.
Even if they do not opt to take up the option to provide ACT or FACT as bundled Medi- Cal services, county FSP programs must deliver ACT and FACT with fidelity and consistent with the requirements established in the BH-CONNECT EBP Policy Guide.
B.4.2 Level 1: Full Service Partnership Intensive Case Management
B.4.2.1 Overview
Intensive Case management (ICM), like the ACT model of care, emphasizes long-term community-and-team-based care for individuals living with significant behavioral health conditions.[84] ICM is more than just case management with referrals; ICM has a small caseload size and is delivered by a multidisciplinary team that provides services and supports based on the unique needs of each client, including peer services, crisis intervention, psychosocial rehabilitation, psychotherapy, medication management, and more.[85],[86] Compared to standard care, ICM has been shown to improve general functioning, employment and housing outcomes, and reduce length of hospital stays.87] While ICM does not have set fidelity criteria like ACT, ICM includes many of the same components including low staff to client ratios, assertive outreach, and direct service delivery.[88],[89] Many current county FSP programs resemble the ICM service model.
The BHSA requires county FSP programs to have an established standard of care based on an individual’s acuity and criteria for step-down into the least intensive level of care. For the purposes of California’s FSP programs, FSP ICM is designed to be the least intensive FSP level of care. FSP ICM will include a comprehensive set of community-based services for individuals with significant behavioral health conditions, delivered through a team-based approach. FSP ICM will look much like the flexible delivery model that is widespread in today’s FSP programs.
Individuals who may appropriately receive FSP ICM may include those who were receiving ACT and have been clinically determined to no longer require the intensity of ACT and be ready to step down in level of care. Individuals who may receive FSP ICM also include those who need moderate to significant levels of support but do not meet clinical eligibility criteria for ACT. FSP ICM is a stand-alone high-intensity mental health service delivery model, and therefore cannot be provided concurrently with ACT or HFW. FSP ICM is appropriate for BHSA eligible individuals living with co-occurring mental health and SUD conditions and for those aged 18-26 or younger who are not connected to children’s services, if determined to be clinically and developmentally appropriate.
B.4.2.2 Full Service Partnership Intensive Case Management Eligibility Criteria
When determining whether FSP ICM is the appropriate level of care, counties and service providers should consider the following:[90]
A current or suspected[91] Diagnostic and Statistical Manual of Mental Disorders (DSM) diagnosis consistent with a serious mental illness (SMI), serious emotional disturbance (SED), SUD, or co-occurring SMI and SUD; AND
A moderate to significant functional impairment, including:
Consistent difficulty performing practical daily tasks needed to function in the community such as maintaining personal hygiene, meeting nutritional needs, caring for personal business affairs, obtaining medical, legal, and housing services, recognizing and avoiding common dangers or hazards to one’s self and one’s possessions;
Persistent or recurrent difficulty performing daily living tasks, except with moderate support or help from others such as friends, family, or relatives;
Difficulty maintaining consistent employment at a self-sustaining level or to carry out homemaker roles; and/or
Difficulty maintaining a safe living situation (e.g., repeated evictions or loss of housing); AND
An indicator of continuous high-service needs, including:
Risk of hospitalization or crisis/emergency care without this service;
Risk of returning to unsheltered homelessness after being placed in interim housing, or risk of returning to homelessness after being placed in permanent supportive housing without this service;
Intractable (persistent or recurrent) severe major symptoms (e.g., affective, psychotic suicidal);
Coexisting SUD of significant duration (greater than 6 months);
High-risk or a recent history of being involved in the criminal justice system;
In substandard housing, homeless, or at at-imminent risk of becoming homeless;
Living in housing, but clinically assessed to need more intensive services to maintain housing;
Living in an inpatient bed or in a supervised community residence, but clinically assessed to be able to live more independently if intensive services are provided; and/or
Inability to participate in traditional office-based services.
As noted above, eligibility criteria for ACT are outlined in the BH-CONNECT EBP Policy Guide; generally speaking, these criteria are similar to FSP ICM but rely on indicators of more significant need, risk, or acuity in comparison to FSP ICM.
B.4.2.3 Full Service Partnership Intensive Case Management Service Components
FSP ICM participants may need some or all of the same services as ACT including, but not limited to:[92]
Assessment
Crisis Intervention[93]
Medication Support Services
Peer Support Services
Psychosocial Rehabilitation
Referral and Linkages
Therapy
Treatment Planning
B.4.2.4 Full Service Partnership Intensive Case Management Team Structure
FSP ICM requires a team-based approach with an identified team lead. FSP ICM teams are required to have a ratio of no more than 25 participants per FSP ICM team lead.
In addition to the required team lead, FSP ICM teams should include a combination of partial and full-time providers such as prescribers, peer support specialists, registered nurses (RNs), and other qualified providers. Counties should align the staffing model with the needs of the individuals receiving services.
FSP ICM teams are expected to provide as many contacts as needed to support an FSP participant’s recovery. In most cases, individuals receiving FSP ICM will need at least one contact a week. Individuals receiving FSP ICM will typically require fewer contacts than individuals receiving ACT, but more contacts than individuals receiving routine outpatient services. Given the intensity of their needs, conducting face-to-face contacts most of the time is recommended, though telehealth may be used judiciously for visits that exceed the once per week threshold. The type and frequency of ICM contacts should be determined based on the needs of each individual and the intensity of the service may be higher than four contacts per month.
B.4.2.5 Aligning Full Service Partnership Intensive Case Management with Medi- Cal
All of the primary FSP ICM service components are billable under Medi-Cal (see “Service Components” above) and should be billed accordingly for Medi-Cal members (i.e., case management plus additional Medi-Cal SMHS on an unbundled basis). In alignment with the “whatever it takes” philosophy, FSP funding can be used for services not covered by Medi-Cal, as needed. This includes outreach and engagement services and consumer-operated services.[94]
For non-Medi-Cal BHSA eligible individuals, FSP funding may be used for service components that commercial health plans do not cover, or for all components for the fully uninsured.
B.4.3 High Fidelity Wraparound
B.4.3.1 Overview
HFW provides a comprehensive, holistic, youth and family- driven way of responding when children or youth experience significant mental health or behavioral challenges.[95] At its core, HFW is defined as adherence to the four phases and ten principles of the HFW model and a team-based and family-centered evidence- based practice that includes an “anything necessary” approach to care for children and youth with the most intensive mental health or behavioral challenges. The HFW model combines a team-based case management and facilitation approach with individualized and community-based mental health services and supports tailored to meet the individualized needs of the youth and family.
In 1997, CA Wraparound was established through Senate Bill 163 to allow counties to provide optional wraparound services to children and youth with child welfare involvement, and is the current model for wraparound delivery in California. The California Department of Social Services (CDSS) over the last several years has invested in ways to improve fidelity to the HFW model, including by aligning CA Wraparound standards with the National Wraparound Initiative’s Wraparound Standards in collaboration with a state Wraparound Steering Committee, and – in partnership with DHCS – designating the UC Davis Resource Center for Family-Focused Practice to conduct approvals and certifications necessary to ensure standards of HFW are met for providers of the Family First Prevention Services Act Part IV aftercare services to ensure compliance with W&I Section 4096.6, subdivision (d)(2).
HFW is not restricted to children and youth receiving foster care or involved with child welfare. DHCS intends to strengthen and complement California's wraparound program by formally implementing HFW as a service within FSP and to support a diverse range of needs and systems interaction.
HFW is regarded as an alternative to out-of-home placement for children with complex needs, by providing intensive services in the family’s home and community. HFW centers family voice and decision-making in developing a care plan to reach desired outcomes by providing a structured, creative, and individualized set of strategies that result in plans/services that are effective and relevant to the child, youth, and family.
When wraparound is delivered consistent with the High Fidelity Wraparound model, there is a strong evidence base for positive impact on youth and families. Studies have found that programs implementing HFW achieve more favorable outcomes, including improved child behavior, mental health functioning, parent satisfaction, and reduced absences and suspensions from school.[96] Supporting youth and families through HFW and keeping the family intact may also help achieve and maintain stable housing outcomes.
Pursuant to the BHSA, county FSP programs must implement HFW beginning in July 2026 (see Full Service Partnership Exemptions for county implementation requirements).[97] In addition, DHCS is clarifying coverage of HFW as a Medi-Cal service bundle within SMHS to meet the goal of delivering care to children and youth that matches their level of need in the least restrictive environment.
By early 2026, DHCS will release detailed guidance to support counties in implementing HFW as a Medi-Cal service to fidelity. DHCS will seeks to make available training, technical assistance, and fidelity monitoring support available to all counties. As county FSP programs work towards delivering HFW with fidelity, counties shall refer to the forthcoming Medi-Cal guidance which may include but not be limited to:
Clinical indicators of need for HFW
HFW team structure requirements
Key functions of HFW teams
Billing Medi-Cal for HFW services delivered to Medi-Cal members[98]
Documentation requirements for HFW teams that bill Medi-Cal
Training and technical assistance requirements
B.4.3.2 Aligning High Fidelity Wraparound in Full Service Partnership with Medi- Cal
Pursuant to the BHSA, counties must bill Medi-Cal for all Medi-Cal-covered services. Through the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit, HFW is covered statewide. As described above, county FSP programs must implement HFW beginning in July 2026. As will be specified in forthcoming Medi-Cal guidance, many of the components of HFW will be Medi-Cal billable on a bundled basis, where applicable.
One element of HFW that is not currently billable to Medi-Cal is “flexible funds,” which can be used by the HFW team for anything determined necessary. The HFW practice model requires timely access to flexible funding to support and address the urgent and individualized needs of children, youth and their families when these needs are not readily met by other resources (i.e., Medi-Cal programs or community-based resources).
Counties may use FSP funding for any service components not covered through Medi- Cal or through other funding sources (e.g., Immediate Needs funds for children/youth in foster care, and Medi-Cal BH-CONNECT Activity Funds for all welfare-involved children and youth). FSP will be an important source of funding for flexible funds, as well as for caregiver respite, when it is unable to be covered as a Community Support through Medi-Cal Managed Care.
For the BHSA eligible fully uninsured, FSP funding may be used for all components.
B.5 Individual Placement and Support Model of Supported Employment
B.5.1 Overview
The Individual Placement and Support (IPS) model of Supported Employment is an evidence-based intervention that engages individuals living with significant behavioral health needs in finding and maintaining competitive employment, which can play a crucial role in their recovery and integration into the community.[99],[100] IPS provides structure, purpose, and social connection and is shown to reduce isolation and combat stigma for individuals living with mental health conditions and SUD.[101]
IPS services can be delivered to an individual as a standalone service or alongside other FSP service models such as ACT, FACT, FSP ICM, and HFW, to offer a comprehensive approach to recovery that addresses both clinical and functional needs. The Evidence Base Practice (EBP) CSC for FEP funded under Early Intervention can also be provided alongside of IPS. Alternately, these FSP EBPs can incorporate flexible employment or education supports for individuals who choose not to pursue full participation in IPS but are interested in some employment or education services.
The IPS model is based on eight core principles:[102]
Competitive Employment
Systematic Job Development
Rapid Job Search
Integrated Services
Benefits Planning
Zero Exclusion
Time-Unlimited Supports
Worker Preferences
In the model, an IPS team provides “pre-employment services,” including vocational assessments, employment planning and job placement, and “employment sustaining services,” which include career advancement support, job coaching, and ongoing follow- along supports.[103]
Pursuant to BHSA, county FSP programs must implement IPS beginning in July 2026 (see Full Service Partnership Exemptions for county implementation requirements). In addition, in December 2024, CMS approved State Plan Amendment (SPA) 24-0051, which establishes IPS as a covered benefit in the Medi-Cal program.[104] Counties have the option to provide IPS as a bundled service with a monthly bundled reimbursement rate under Medi-Cal in the Medi-Cal SMHS, Drug-Medi-Cal (DMC), and Drug- Medi-Cal Organized Delivery System (DMC-ODS) delivery systems beginning in 2025.
Counties should use the BH-CONNECT EBP Policy Guide to support implementation of IPS. The EBP Policy guide includes information about the evidence-based service criteria for IPS, staffing structure for teams of behavioral health practitioners delivering IPS, and other best practices for delivering IPS with fidelity to the evidence-based model.
In addition, all counties must adhere to the training, technical assistance and fidelity requirements identified in the forthcoming BH-CONNECT EBP BHIN. The BH-CONNECT EBP BHIN also includes coverage, payment and other compliance requirements for counties that elect to cover IPS in Medi-Cal.
For counties that do not intend to deliver IPS as covered Medi-Cal services, find details about delivery and billing for IPS through FSP programs only below.
B.5.2 Aligning Individual Placement and Support Model of Supported Employment in Full Service Partnership with Medi-Cal
Pursuant to BHSA, counties must bill Medi-Cal for all Medi-Cal-covered services. As described above, beginning in 2025 counties have the option to cover IPS as a bundled Medi-Cal service. Counties that opt to deliver IPS as a Medi-Cal service will be eligible for a monthly reimbursement rate intended to fully support the cost of operating an IPS team. Counties that do not choose to offer IPS as a bundled Medi-Cal service are still required to bill Medi-Cal for unbundled IPS services provided to Medi- Cal members.
These services may include the following SMHS:
Psychosocial Rehabilitation
Referral and Linkages
Treatment Planning
Even if they do not opt to take up the option to provide IPS as a bundled Medi-Cal service, county FSP programs must deliver IPS with fidelity and consistent with the requirements established for BH-CONNECT.
For non-Medi-Cal BHSA eligible individuals, FSP funding may be used for components commercial health plans do not cover, or for all components for the fully BHSA eligible uninsured.
B.6 Assertive Field-Based Initiation for Substance Use Disorder Treatment Services
B.6.1 Overview
DHCS, in partnership with its counties, remains committed to expanding lifesaving care to individuals living with a SUD. DHCS and counties have worked to build and strengthen access to SUD treatment, particularly medications for addiction treatment (MAT), for individuals with opioid, alcohol, and stimulant misuse and use disorders in particular. Beyond traditional treatment settings and approaches, which only reach a small percentage of people living with SUDs, DHCS recognizes that more proactive strategies are needed to engage, prevent overdose, and improve access to MAT for most individuals living with SUD who remain unengaged in care.[105] Pursuant to the Behavioral Health Services Act (BHSA) and in accordance with W&I Code section 5887, subdivision (a)(3), counties will be required to deploy assertive field-based initiation programs that proactively engage individuals living with SUD and offer low barrier access to MAT.
Assertive field-based initiation promotes a proactive “no-wrong door” approach to connect more individuals living with SUD to MAT on a voluntary basis, similar to assertive, field-based models that promote proactive engagement and treatment of individuals living with Serious Mental Illness (SMI). Assertive field-based initiation is focused on providing rapid access to MAT and connection to services for individuals at the highest risk of overdose. Counties are encouraged to identify these populations, including those who are unhoused/housing insecure, justice-involved and/or those with co-occurring mental health needs. Assertive field-based initiation requires counties to conduct ongoing, targeted outreach to engage and initiate individuals living with SUD into MAT in any community based and low barrier setting. Community based low barrier settings include the street, shelters, homeless encampments, consumer-operated wellness centers, drop-in centers, syringe service programs, medication and mobile Narcotic Treatment Programs (NTPs), and other easily accessible locations that aim to reach people where they are.
B.6.2 Assertive Field-Based Programmatic Requirements
Counties are required to provide rapid access to all Food and Drug Administration (FDA) approved MAT by strengthening existing and/or standing-up at least one initiative in each of the following three areas that comprise their assertive field-based programs:
Data-informed, targeted outreach on an ongoing basis to BHSA-eligible individuals with SUD needs to engage them in SUD services, including MAT, if needed.
Mobile field-based programs.
Open-access clinics.
Counties’ assertive field-based programs are required to serve BHSA-eligible individuals living with SUD treatment needs and prioritize those who are at higher risk of overdose, including those known to have experienced overdose reversals, or who are experiencing homelessness and/or justice-involvement. Best practices include establishing coordinated surveillance and overdose identification systems with local emergency medical services, emergency departments, and public health authorities for rapid (e.g., daily or weekly) referrals to post-overdose follow-up teams.
Counties are also required to strategically locate their assertive field-based outreach and program models in settings where significant numbers of individuals living with SUD are located and/or areas with high rates of overdose reversals, which may include hospital Emergency Departments (EDs), homeless encampments, interim housing and permanent supportive housing units set aside for people formerly living in homeless encampments, syringe services programs, jails, and other identified areas.
Counties are encouraged to work with existing assertive field-based programs — defined as outreach, mobile field-based programs, including street medicine providers, and open access clinics — to meet the programmatic requirements detailed in this section. Counties can also strengthen existing initiatives and/or stand-up one comprehensive initiative that conducts data-informed, targeted outreach on an ongoing basis to BHSA-eligible individuals with SUD needs; operates mobile field-based program(s); and works out of open-access clinic(s). For example, under this approach, a county can work with a low barrier “brick and mortar” (e.g., consumer-operated wellness centers) or drop-in SUD clinic to establish mobile outreach teams that visit homeless encampments, interim housing and permanent supportive housing to engage individuals in SUD care, initiate and maintain MAT. Counties must ensure all of their field-based assertive initiation programs comply with existing confidentiality requirements.
The requirements in this section are designed to allow counties to build upon existing field-based SUD programs to the extent that they already offer them. DHCS recognizes counties may be at different levels of readiness to comply with assertive field-based initiation requirements. Some counties may already have SUD field-based programs in place that meet or are close to meeting DHCS’ requirements by July 1, 2026. Other counties may require additional effort and support to meet DHCS’ requirements. As a result, DHCS is offering counties flexibility to gradually meet assertive field-based initiation requirements over a three-year time frame from July 1, 2026, to July 1, 2029. Counties will be required to describe their approach for meeting assertive field-based initiation for SUD treatment requirements in their Integrated Plans.
Promising and Best Practices
Counties are encouraged to promote a person-centered approach in their assertive field-based initiation programs to provide access to lifesaving care, prevent overdose and improve the quality of life for individuals living with SUDs. Assertive field-based programs are encouraged to provide the following activities:
Harm Reduction. Share harm reduction supplies, such as harm reduction kits with naloxone, as well as testing strips (including but not limited to fentanyl and xylazine testing strips).
Primary Care. Provide individuals with necessary wound care, Hepatitis C and Human Immunodeficiency Virus (HIV) testing and care.
Post-Overdose Follow-Up Engagement Services. Provide post-overdose follow-up engagement services as part of their assertive field-based programs (e.g., through targeted outreach or mobile field-based programs). When programs become aware that someone has survived an overdose, including through dedicated communication and coordination channels for this purpose, teams can conduct immediate community-based outreach (e.g., within 72 hours) after the known overdose and provide supports, education and facilitate rapid access to MAT. This approach has been successfully piloted in California counties like San Francisco[106] and in other states, such as West Virginia,[107] New Jersey,[108] and Oregon.[109]
Access to Peer Support Specialists. As individuals with lived experience, peers personally understand the experience of the individuals they serve and can help clarify the most effective set of services for each individual’s needs.
Counties may also collaborate to establish targeted outreach programs, field-based mobile teams, and open-access clinics to maximize resources and leverage geographic efficiencies to expand rapid access to MAT for individuals residing in adjoining counties. For example, under a cross-county collaboration approach, counties may pool together financial resources to design and support:
Mobile field-based programs, such as street outreach programs with an embedded prescriber or mobile NTPs, to rotate through locations across multiple counties on designated days.
Open-access clinics, to provide care and accept MAT referrals for individuals residing in partnering counties.
B.6.2.1 Rapid Access to Medications for Addiction Treatment
Counties are required to ensure that their outreach initiatives aim to reach priority populations who can benefit from MAT and mobile field-based programs and open- access clinics are able to provide rapid access for all Food and Drug Administration (FDA)-approved MAT and other medications clinically effective at treating alcohol, tobacco, opioid, and stimulant use disorders directly or through referrals. County field-based programs are expected to work toward ensuring same day MAT access, inclusive of leveraging existing initiatives that may sit outside of county behavioral health. Medication choice shall be individualized and tailored to the individual’s clinical condition rather than based solely on availability. County field-based programs that are not certified to dispense methadone must provide referrals to NTPs, medication units, mobile NTPs, and EDs to rapidly initiate methadone.[110] Best practice is to follow-up with the individual to help ensure enrollment with the provider for continuing care.
To meet this requirement, field-based programs can employ or contract with MAT prescribers directly or refer individuals to providers who are able to rapidly initiate all FDA approved MAT, including CA Bridge programs, Federally Qualified Health Centers (FQHCs), Tribal Health programs, NTPs and medication units. Counties can also utilize telehealth models to facilitate rapid initiation of MAT. For individuals initiated on MAT, county field-based programs must provide or refer individuals to other programs for MAT maintenance. Counties must work to ensure all recovery-oriented services, including behavioral therapies and counseling, from MAT providers are accessible by individuals.
Counties will be required to detail how and when they will be able to assure same day access to MAT, inclusive of leveraging existing initiatives that may sit outside of county behavioral health, and plans for medication continuation in their initial Integrated Plan. Counties that cannot assure same day access to MAT effective July 1, 2026, will be required to work towards providing same day access to MAT as detailed in their Integrated Plans by July 1, 2029.
B.6.2.2 Targeted Outreach
Counties will be required to conduct ongoing, targeted outreach to connect individuals with SUD services, including MAT, in accordance with W&I section 5806, subdivision (a)(2). Mobile field-based programs, open-access clinics, or other providers (e.g., Full Service Partnership) can conduct ongoing targeted outreach to priority populations.
Ongoing, targeted outreach services may be performed by new or existing mobile field- based teams (described below) or may be delivered through other models, such as a case management team embedded within a clinic that conducts outreach services, or case management teams supporting individuals living in interim housing and/or permanent supportive housing.
Recommended Best Practices
To identify the highest-need outreach locations, counties are encouraged to collaborate with Emergency Medical Services (EMS), law enforcement, managed care plans (MCPs), health systems and hospitals, FQHC/RHS’, individuals with living or lived experience, and other partners to obtain data on regions and populations with high rates of overdose, overdose reversals, drug-related arrests, and other relevant statistics on a regular basis.
B.6.2.3 Mobile Field-Based Programs
Mobile field-based programs leverage teams to conduct “on the ground” field-based outreach to provide engagement, harm reduction support, trust building, motivational interviewing, and directly provide or facilitate rapid access to MAT and other SUD services. Counties can determine the composition of the mobile teams. Programs can rotate team members, who can include behavioral health providers (e.g., social workers, SUD counselors), peer support specialists, community health workers, nursing staff, physicians, and physician extenders. At a minimum, the mobile field-based teams must guarantee quick access to FDA-approved MAT, by embedding MAT prescribers or referring individuals to prescribers, including NTPs to ensure access to methadone.
Counties can work with existing mobile field-based programs across other delivery systems, including street medicine providers, and/or stand up new mobile field-based programs to facilitate rapid access to MAT directly or through referrals for all FDA- approved MAT. Mobile field-based models that counties can utilize to meet requirements include:
Street Medicine Providers. Counties may contract with street medicine providers to provide mobile field-based assertive initiation services. Street medicine refers to a set of health and social services developed specifically to address the unique needs and circumstances of individuals experiencing unsheltered homelessness, delivered directly to them in their own environment per All Plan Letter (APL) 24-001.[111] Street medicine providers may include primary care providers such as licensed medical providers (e.g., Doctor of Medicine (MD)/Doctor of Osteopathic Medicine (DO), Physician Assistant (PA), or Nurse Practitioner (NP)) who may prescribe MAT to people experiencing unsheltered homelessness. DHCS highly encourages MCP and county collaboration and coordination for street medicine related initiatives.
Street Outreach Programs with MAT Prescribers. Street outreach focused on individuals experiencing homelessness is typically conducted by a mobile multidisciplinary team, which can include a psychiatrist, a nurse care manager, social workers, peer support specialists, community health workers and outreach workers with behavioral health expertise, including individuals with lived experience. The team can provide street-based behavioral health care, including evaluation, assessment, and treatment with medications provided directly in the field such as MAT; teams can also refer individuals to NTPs for methadone.
Mobile NTPs. A mobile NTP delivers MAT in the field, including methadone, outside of the four-walls of an NTP clinic setting. A mobile NTP operates from a motor vehicle that serves as a mobile component (conveyance) and is operating under the registration of the NTP, and engages in maintenance and/or detoxification treatment with narcotic drugs in schedules II-V, at a location or locations remote from, but within the same state as, its registered location. Operating a mobile NTP is a coincident activity of an existing NTP.[112] Effective July 28, 2021, the federal Drug Enforcement Administration (DEA) allows DEA registered, Substance Abuse and Mental Health Services Administration (SAMHSA) certified, and DHCS licensed NTPs to operate mobile NTPs that dispense methadone and buprenorphine if they meet federal, state, tribal, and local requirements. Health and Safety Code (HSC) section 11839.6.1 authorized DHCS to regulate and establish a program for the operation of mobile NTPs. Effective January 4, 2024, DHCS issued Behavioral Health Information Notice (BHIN) 24-005 to implement mobile NTPs in California. This BHIN sets forth the minimum requirements that a mobile NTP shall comply with to lawfully operate in California.[113]
B.6.2.4 Open-Access Clinics
Counties will be required to support open-access clinics, which are outpatient settings providing low barrier, low-threshold rapid access to MAT. Open-access clinics must directly provide or refer to the most appropriate form of MAT, including methadone. CA Bridge Sites located in EDs can refer individuals initiated on MAT to open-access clinics for ongoing MAT care.
To meet open-access program requirements, counties can leverage existing or stand-up new “brick and mortar” programs within their catchment areas to provide rapid access to MAT. Open-access clinic models that counties can utilize include:
Syringe Services Programs with Drop-in Clinic Services. Syringe services programs provide harm reduction services to individuals with SUD and some offer clinic services for individuals who drop-in across California. Programs provide sterile syringes, naloxone, wound care and first aid; testing for HIV and hepatitis C; conduct overdose education; and directly provide or refer individuals to MAT, SUD and mental health treatment, as well as housing services and employment services. Syringe services programs often provide food, drinks, clothes, showers, and other basic supplies to support individuals experiencing or at risk of homelessness. Programs are located in a variety of settings, including churches, health departments and store fronts, and may provide home delivery.[114]
Medication Units. Licensed NTPs can establish medication units to dispense methadone and other MAT in community sites such as FQHCs, drop-in centers and county health departments.[115]
Drop-in Outpatient Clinics with Open-Access Scheduling. Counties can also support outpatient drop-in clinics across a range of providers, including FQHCs, community mental health centers, NTPs, hospital outpatient clinics (e.g., ambulatory outpatient CA Bridge Sites) and Indian Health Care Partners, where patients can be seen on the same day they “drop-in” or request to be seen. Outpatient clinics are highly recommended to provide primary care, MAT, and behavioral health treatment, as well as care coordination.
B.6.3 Integrated Plan Requirements
All counties are required to include their assertive field-based implementation plans in their Integrated Plans. County Integrated Plans must describe county approaches and timelines for meeting assertive field-based requirements, including ensuring rapid access to medications for addiction treatment (MAT), conducting targeted outreach, and supporting mobile field-based and open-access programs.
B.6.4 Substance Use Disorder Primary Full Service Partnership Option
Senate Bill (SB) 326 does not prohibit counties from establishing FSP programs for individuals with primary substance use disorder (SUD) diagnoses (i.e., without co-occurring significant mental health needs). However, counties are not required to develop new, dedicated FSP Levels of Care specific to SUD.[116] Counties are also not required to establish FSPs that are exclusively for SUD, apart from implementing new, assertive field-based initiation of SUD care requirements. As described in Chapter 7, Section B.3.5 Full Service Partnership Co-Occurring Capabilities, county FSP programs will be expected to be co-occurring capable and be equipped to provide comprehensive care to eligible individuals living with co-occurring significant behavioral health needs and SUD.
C. Housing Interventions
C.1 Housing Interventions Funding
Counties are required to use 30 percent of the funds distributed by the State Controller’s Office into their Behavioral Health Services Fund (BHSF) for Housing Interventions.
Of the funding distributed to counties for Housing Interventions:
50 percent must be used to support the housing needs of individuals who are chronically homeless, with a focus on those in encampments.
Up to 25 percent may be used for capital development projects.
If a capital development project identifies chronically homeless individuals as a priority population, the project funding will contribute toward the 50 percent requirement.
C.2 Introduction and Background
Using the Behavioral Health Services Act (BHSA) Housing Interventions funding, counties can develop an ongoing behavioral health housing program to increase access to permanent supportive housing for people meeting BHSA eligibility who are chronically homeless, experiencing homelessness, or are at risk of homelessness.
These policies have been developed to give counties flexibility so that each community can develop a program that is reflective of its needs. The flexibilities of Housing Interventions are also intended to build upon other housing initiatives, including but not limited to Homekey+, Behavioral Health Bridge Housing (BHBH), No Place Like Home (NPLH), Homekey, Project Roomkey, the Community Care Expansion (CCE) Program, the Housing and Homelessness Incentive Program (HHIP), the Encampment Resolution Fund (ERF), and the Homeless Housing Assistance and Prevention Grant Program (HHAP). Housing Interventions are also intended to complement CalAIM Community Supports and Transitional Rent available through Medi-Cal Managed Care Plans (MCPs). The Transitional Rent benefit available through MCPs specifically to seamlessly connect BHSA eligible individuals receiving Transitional Rent to BHSA-funded Housing Interventions.
In the following sections, the Department of Health Care Services (DHCS) identifies a number of policies and procedures that counties must develop to support the implementation of Housing Interventions. Those policies and procedures are not subject to approval by DHCS but must be provided to DHCS upon request.
C.3 Program Priorities
The development of Housing Interventions has been driven by the following priorities:
Reduce homelessness among BHSA eligible individuals experiencing homelessness with a behavioral health condition, focusing efforts on the chronically homeless, with a focus on those in encampments.
To the extent possible, provide individuals with permanent supportive housing, including voluntary, flexible, and intensive supports and services available such as Assertive Community Treatment, Intensive Case Management, and other supports funded under the BHSA and Medi-Cal consistent with best practice.
Provide flexibility for counties to respond to local conditions and needs, and to innovate.
Provide individuals receiving Housing Interventions access to clinical and supportive behavioral health services.
Support the provision of low-barrier, harm reduction, and Housing First principles.
Complement ongoing state, county, city, Continuum of Care, and tribal efforts to address homelessness, including but not limited to those provided through Medi-Cal.
C.4 Eligible and Priority Populations
C.4.1 Eligible Populations for Housing Interventions[117]
Individuals must meet the BHSA eligibility requirements, identified in this policy manual[118] and meet the definition of:
C.4.1.1 Experiencing Homelessness and At Risk of Homelessness
W&I Code section 5892, subdivision (k)(3) provides that for purposes of the BHSA, “experiencing homelessness or at risk of homelessness” means people who are homeless or at risk of homelessness as defined by 24 CFR section 91.5 or as otherwise defined by the State Department of Health Care Services for purposes of the Medi-Cal program.
For purposes of the BHSA, DHCS is adopting the definitions of experiencing homelessness and at risk of homelessness consistent with CalAIM Community Supports, which are the same as the definitions provided at 24 CFR section 91.5 with three modifications, as follows:
Individuals exiting an institution or carceral setting are considered homeless if they were homeless immediately prior to entering that institutional or carceral stay or become homeless during that stay, regardless of the length of the institutionalization or incarceration.
The timeframe for an individual or family who will imminently lose housing is extended from 14 days for individuals considered homeless and 21 days for individuals considered at-risk of homelessness to 30 days.
An individual or family is not required to have an annual income below 30 percent of median family income for the area.
Additionally, anyone who was homeless or at risk of homelessness prior to the receipt of Transitional Rent (as covered by a Medi-Cal managed care plan) or prior to the receipt of housing funded by MHSA is considered homeless for BHSA purposes.
C.4.1.2 Chronically Homeless
W&I Code section 5892, subdivision (k)(2) provides that for purposes of the BHSA, “chronically homeless” means an individual or family that is chronically homeless as defined in 42 U.S. Code section 11360 or as otherwise modified or expanded by the State Department of Health Care Services.
DHCS is adopting the Department of Housing and Urban Development (HUD) definition of chronic homelessness, identified under 24 CFR section 91.5 with two modifications, as follows:
The requirement that a discontinuous period of 12 months of homelessness over the last three years occur on at least four separate occasions is eliminated; any number of occasions will suffice so long as the combined duration equals at least 12 months.
Consistent with the Medi-Cal modification to the definition of "homeless,” anyone residing in an institutional care facility, defined according to the HMIS definition of “institutional situations,” who was chronically homeless prior to entry retains that status upon discharge, regardless of length of stay.
Additionally, anyone who was chronically homeless prior to the receipt of Transitional Rent or prior to the receipt of housing funded by MHSA and is transitioning from either of these services to Housing Interventions services will be considered chronically homeless under Housing Interventions.
Regarding the requirement that 50 percent of Housing Interventions be directed to individuals experiencing chronic homelessness, the determination that an individual meets the definition of chronically homeless will be made by counties at enrollment and may maintain their status as such for the duration of their enrollment in Housing Interventions services.
C.4.1.3 People in Encampments
The BHSA requires that 50 percent of a county’s Housing Interventions funds be used for Housing Interventions for persons eligible for BHSA funding who are chronically homeless, “with a focus on those in encampments.”[119] The BHSA definition for encampments is in alignment with the Department of Housing and Urban Development (HUD)[120] definition. An encampment includes the following:
A group of people sleeping outside in the same location for a sustained period.
The presence of some type of physical structures (e.g., tents, tarps, lean-to’s).
The presence of personal belongings (e.g., coolers, bicycles, mattresses, clothes).
The existence of social support or a sense of community for residents.
Counties are expected to prioritize serving individuals living in encampments with methods consistent with the U.S. Interagency Council on Homelessness’ 19 Strategies for Communities to Address Encampments Humanely and Effectively. It is essential that counties provide Housing Interventions services that are relevant and responsive to the needs of individuals in encampments who are chronically homeless and are BHSA eligible, including the provision of housing and behavioral health interventions that will help individuals transition out of encampments and into permanent supportive housing.
C.4.2 Priority Populations
In addition to specifying the populations who are eligible for Housing Intervention services (“Eligible Populations”), the BHSA identifies a smaller subset of populations who should be prioritized for BHSA services (see BHSA requirements here).
Priority Populations[121]:
Children and youth in the Eligible Population who also satisfy one of the following:
In, or at risk of being in, the juvenile justice system;
Reentering the community from a youth correctional facility;
In the child welfare system; or
At risk of institutionalization.
Adults or older adults in the Eligible Population who also satisfy one of the following:
In, or are at risk of being in, the justice system;
Reentering the community from prison or jail;
At risk of conservatorship; or
At risk of institutionalization.
C.4.3 Individuals Transitioning from MHSA to BHSA
For individuals housed under the MHSA as of June 30, 2026, the following policies apply:
Counties may transfer individuals housed in permanent housing directly to BHSA-funded Housing Interventions without eligibility redetermination.
Individuals receiving interim housing under the MHSA who are not enrolled in an MCP may also be transferred to BHSA Housing Interventions without eligibility redetermination.
For individuals in interim housing who are in an MCP, the county should connect the individual to their MCP for assessment of eligibility for Transitional Rent. The goal is for this to be seamless to the individual being served. This will require the delivery systems to put processes in place for effective coordination.
Those determined eligible for Transitional Rent may be transferred to the MCP and may not receive rental assistance or housing under BHSA Housing Interventions until they are no longer eligible for Transitional Rent.
Those determined ineligible for Transitional Rent may be transferred directly to BHSA Housing Interventions without eligibility redetermination.
Anyone who was chronically homeless when housed under MHSA, and who was transferred from MHSA to BHSA, will be considered chronically homeless for purposes of the requirement to direct 50 percent of Housing Interventions to individuals who are chronically homeless.
C.5 Program Requirements
In addition to the eligibility requirements, W&I Code section 5830, subdivision (a) specifies the following:
Housing Interventions shall not be limited to individuals enrolled in either a Full Service Partnership or Medi-Cal.
Counties shall not discriminate against or deny access to housing for individuals that are utilizing medications for addiction treatment or other authorized medications, or individuals who are justice-involved.
Housing Interventions shall comply with the core components of Housing First, as defined in subdivision (b) of W&I Code section 8255, and may include recovery housing. See additional information in the Chapter 7, Section C.9.5.1 Housing First below.
All Housing Interventions settings must be combined with access to clinical and supportive behavioral health care and housing services that will promote the individual’s health and functioning and long-term stability. Access does not necessitate co-location. Housing Interventions may not be used for behavioral health services; however, these activities can be covered under Behavioral Health Services and Supports or other behavioral health funding sources.
Counties may utilize up to 7 percent of Housing Intervention funds on identified Outreach and Engagement activities. If Housing Intervention funds are used for Outreach and Engagement activities under the Housing Intervention component, counties must adhere to transfer requirements, including required documentation, in Chapter 7, Section C.6 Transfers and Exemptions.
C.6 Transfers and Exemptions
C.6.1 Transfers
Beginning in Fiscal Year 2026, counties may request to transfer funds distributed to the counties Behavioral Health Services Fund to spend more than or less than 30 percent of their local BHSF on Housing Interventions.[122] Please refer to the Funding Transfer Requests section for more information.
Transfer of funds into or out of Housing Interventions funds does not relieve the county from complying with:
The requirement to use 50 percent of Housing Interventions funds on services for the chronically homeless.
The requirement to use no more than 25 percent of Housing Interventions funds on capital development projects.
C.6.2 Exemptions
State law permits counties to request exemptions to Housing Interventions spending requirements. Exemptions are necessary for counties requesting a funding adjustment beyond the 7 percent allowed through the transfer process. Counties with a population of less than 200,000 may request exemptions beginning with the 2026-29 Fiscal Years’ county Integrated Plan (IP), and all counties regardless of size may do so beginning with the 2032-35 Fiscal Years’ county IP. Exemption requests must be submitted as part of the draft IP due by March 31st of the year prior to the fiscal years the IP covers. Counties must also include a letter from the County Administrative Officer approving the draft IP, including exemption requests. Exemption requests are subject to DHCS approval; counties may request exemptions from one or more of the following requirements[123]:
30 percent of the BHSF funds distributed to the county for Housing Interventions services.
50 percent of the county’s Housing Interventions funds on those who are chronically homeless.
No more than 25 percent of Housing Interventions funds on capital development projects.
Table C.6.2.1 Criteria for Housing Exemption Requests
Requirement | Exemption Request Criteria |
30 percent of BHSF for Housing Interventions | Criteria for increased/reduced percentage (beyond transfer allowance):
Requests for exemptions must include information and data demonstrating that the exemption request criteria provided above are met (e.g., Point in Time Count (PIT), Housing Inventory Count (HIC), HMIS data, Coordinated Entry System data, Electronic Health Record data, etc.). |
50 percent of the county’s Housing Intervention funds on persons who are chronically homeless
| Criteria for reduced percentage:
Requests for exemptions must include information and data demonstrating that the exemption request criteria provided above are met (e.g., PIT, HIC, HMIS data, Coordinated Entry System data, Electronic Health Record data, etc.). |
No more than 25 percent of the county’s Housing Intervention funds on capital development projects | Criteria for increased percentage:
Requests for capital development exemptions must include documentation demonstrating that the exemption request criteria provided above are met (e.g., a detailed budget with funding breakdown, partnership agreements/letters of support, evidence of need for housing production, and other supporting data). |
C.7 Relationship to Medi-Cal Funded Housing Services
Per W&I Code section 5830, subdivision (c)(2), Housing Interventions may not be used for housing services covered by Medi-Cal Managed Care Plans (MCP). Accordingly, counties must work closely with MCPs to ensure that Housing Interventions funds are used to complement, not supplant, MCP-covered services. By working closely with MCPs to coordinate the delivery of housing-related Community Supports covered by MCPs prior to expending the BHSA Housing Interventions funding, counties and MCPs will play a key role in the prudent stewardship of taxpayer dollars and help ensure that funding sources other than the BHSA also contribute to meeting the housing-related needs of BHSA eligible Californians with behavioral health conditions. This statutory requirement will maximize the total amount of the BHSA Housing Interventions funding available to counties, allowing these dollars to go further to improve outcomes for Californians. The close coordination will also facilitate appropriate referrals to additional Community Supports, Enhanced Care Management, and other services delivered by MCPs.
C.7.1 Prohibition on Housing Interventions Coverage of Managed Care Plan-Covered Services
Housing Interventions “shall not be used for housing interventions covered by a Medi-Cal Managed Care Plan.”[124] Under CalAIM, MCPs are authorized to cover five housing-related “Community Supports”[125],[126]:
Table C.7.1. Coverage of Housing-related Community Supports
Service | |
Housing Deposits | Covered by all MCPs in all counties |
Housing Transition Navigation Services | Covered by all MCPs in all counties |
Housing Tenancy and Sustaining Services | Covered by all MCPs in all counties |
Recuperative Care | Varies by MCP |
Short-Term Post-Hospitalization Housing | Varies by MCP |
Transitional Rent[129] | All MCPs required to cover for the behavioral health population beginning January 1, 2026 |
Housing Interventions may not be used to cover any of the services identified above when the individual is eligible for the service through their MCP. BHSA funding can be used if the MCP is not offering the Community Support in a county or if the individual has expended a benefit with a timeline restriction (e.g., the six month aggregate annual cap across Transitional Rent, Short-Term Post-Hospitalization Housing, and Recuperative Care; the limitation of six months per demonstration period for Transitional Rent). Additionally, if a Medi-Cal member is receiving housing services from their MCP, this does not preclude the individual from receiving simultaneous Housing Interventions not covered by the MCP. For example, an individual who is receiving Transitional Rent could also receive utility assistance funded by the BHSA Housing Interventions because Transitional Rent will only cover landlord-paid utilities that are part of rent, not utilities that the tenant is responsible for paying separately.
C.7.2 Expectations for Coordination with MCPs
Counties will be expected to coordinate closely with MCPs to:
Ensure that Housing Interventions are not used for services that are covered by the MCP.
Support seamless connections from the county to the MCP for coverage of housing services and vice versa.
Provide whole-person care and integrated housing services for MCP-enrolled members with significant behavioral health needs who meet BHSA eligible criteria.
At a minimum, counties are required to establish detailed policies and procedures for issuing referrals to MCPs for housing-related Community Supports (including Transitional Rent) in alignment with forthcoming DHCS guidance and receiving referrals for BHSA Housing Interventions services (guidance forthcoming). DHCS may provide additional information in the future regarding minimum standards for coordination with MCPs regarding housing-related Community Supports and the BHSA Housing Interventions funding.
In addition, counties are strongly encouraged to participate as providers of housing-related Community Supports covered by MCPs, including but not limited to: Transitional Rent, Housing Deposits, Housing Transition Navigation Services, and Housing Tenancy and Sustaining Services in particular. The BHSA Housing Interventions funding is intended to serve as a permanent rental subsidy for housing following MCP-covered Transitional Rent for BHSA eligible individuals, providing seamless continuity and supporting Californians with behavioral health conditions in achieving long-term housing sustainability. As such, it is critical to ensure that counties and MCPs work in full partnership to connect individuals to Transitional Rent and integrate this service with specialty behavioral health services. To that end, DHCS is designing a comprehensive policy approach to standardize processes and streamline requirements for the Transitional Rent benefit with the goal of directly enabling counties to serve as MCP-contracted providers of Transitional Rent and other housing-related Community Supports. Such arrangements will amplify MCP-county coordination of housing-related services and improve the experience of individuals receiving these supports.
C.8 Flexible Housing Subsidy Pools
While not required, Flexible Housing Subsidy Pools (“Flex Pools”) are a strategy to support local partners, including counties, in braiding complementary funding sources and resources to provide permanent supportive housing. Flex Pools provide a model for administering and coordinating multiple streams of funding for rental subsidies and a model which shows potential for the coordination and administration of housing supports. This model for housing payments could facilitate the centralized deployment of housing location, navigation, and rental subsidy payments and supports administrative billing functions. With a Flex Pool, a centralized administrative entity can efficiently connect individuals to the units that best meet their needs from with collective ”housing pool”. Flex Pools provide a solution to create economies of scale, reduce the burden of subsidy administration, and braid together resources seamlessly so that members are accessing housing more quickly and efficiently, and ensures individuals who become housed, remain housed.
Technical assistance will be made available on the use of Flex Pools to coordinate the administration of the BHSA Housing Interventions, housing-related Community Supports (including Transitional Rent), and other sources of housing support funding.
C.9 Allowable Expenditures and Related Requirements
Housing Interventions may be used for the following expenditures and are subject to the identified program requirements as discussed in the remainder of this chapter, which is organized as follows:
Rental Subsidies
Operating Subsidies
Allowable Settings
Other Housing Supports
Landlord Outreach and Mitigation Funds
Participant Assistance Funds
Housing Transition Navigation Services and Tenancy and Sustaining Services
Outreach and Engagement (up to 7 percent)
Other Housing Interventions Requirements
Capital Development Projects
C.9.1 Rental Subsidies
The terms rental subsidies and rental assistance as used in the manual are inclusive of multiple, specific types of rental assistance described in detail in this section. The intent of Housing Interventions is to place and sustain individuals in permanent housing settings including permanent supportive housing developed through the Homekey+ program and other state and locally funded supportive housing programs. While counties may establish short and medium-term rental assistance programs, particularly in interim settings as described below, the goal is to provide rental subsidies in permanent settings to eligible individuals for as long as needed, or until the individual can be transitioned to an alternative permanent housing situation or rental subsidy source. Rental subsidies can be established either as scattered-site (multiple locations) or project-based assistance (one location), including master leasing. Counties are encouraged to work with housing providers in their regions to prioritize the BHSA Housing Interventions for projects serving BHSA eligible individuals within their regions.
C.9.1.1 Rental Assistance Requirements
All rental subsidies must be issued directly to property owners, managers, or providers contracted to administer BHSA-funded rental assistance.
Counties opting to provide rental subsidies must develop policies and procedures that, at a minimum, address the following:
The setting in which the rental subsidy will be used (see Allowable Settings, below).
The duration of payments (to be determined based on individual need and, to the extent possible, to continue as long as necessary or until an alternative subsidy or arrangement is in place).
The calculation of rental assistance for permanent settings. The method elected must use either the rent reasonableness methodology or Fair Market Rents[130] (FMRs), to calculate allowable rental rates. Rent Reasonableness assesses rent based on similar unassisted units in the local area, considering factors like location, size, type, quality, and amenities. It adapts to the actual market dynamics and can be more accurate for specific neighborhoods or property types.
The calculation and types of utilities that are allowed (e.g., electricity, natural gas, water, sewer services, trash collection and internet).
The calculation of individual contribution towards rent. Counties may establish individual contribution requirements of zero to 30 percent of individual income, and the individual contribution requirements may vary by program or setting.[131] Importantly, BHSA-eligible individuals may not be denied Housing Interventions assistance due to lack of income (i.e., if income is zero, tenant pays zero). DHCS recommends 30 percent of adjusted income for permanent settings to match federal vouchers.
The housing-related supportive services and resources that will be made available to individuals who are receiving rental subsidies that will remove barriers and help them obtain and/or maintain supportive housing.
Fraud prevention measures, along with a designated and regular audit process.
Record-keeping methods, including the process for the documentation of all payments issued.
These policies and procedures are not subject to review and approval by DHCS but must be provided to DHCS upon request.
C.9.1.2 Project-Based Housing Assistance
Project-Based Housing (PBH) assistance is a form of rental assistance that is tied to a particular housing unit. PBH differs from tenant-based rental assistance, which is a subsidy or federal voucher assigned to the program participant, and which may relocate with the participant to another unit if needed. PBH can occur in unit(s) of an apartment complex, duplex, triplex, or other structure that is leased, purchased, and/or otherwise subsidized for the purpose of providing housing to eligible individuals. Counties are encouraged to work with housing providers in their region constructing permanent supportive housing and other affordable housing for the eligible population to assess opportunities for project-based rental subsidies, especially through the Homekey+ program. Counties are also encouraged to assess the full pipeline of permanent supportive housing and affordable housing being built within their region so that this funding can be paired with eligible projects that meet the housing needs of BHSA priority populations.
In addition to the policies required for all rental assistance projects (See “Rental Assistance Requirements” section), counties providing PBH are responsible for ensuring policies and procedures governing such units, such as a property management guide for each property meet the requirements identified under “Program Requirements.” The property management guide must also include tenant selection and occupancy procedures (for example, rent contributions, if any; and other core program and fiscal policies to be required by DHCS).
C.9.1.3 Master Leasing
A master lease is a legal agreement through which a master tenant (the county or its subcontracted provider or county grantee) leases a unit or multiple units from a property owner, and then subleases units to subtenants. Under a master lease strategy, the county or subcontracted provider enters into a lease with the property owner, specifying the county/property owner roles and responsibilities, including tenant selection and responsibility for damage and repair. The county then would serve as a master tenant, and then enter into subleases or occupancy agreements with individual(s) who are eligible for Housing Interventions.
Master leasing can be used by counties to provide scattered-site or PBH. Units can include but shall not be limited to single and multi-family homes, apartments, and other privately owned properties.
C.9.2 Operating Subsidies
Housing Interventions allows the use of funds for operating subsidies for either new or existing housing on the allowable settings list provided below. Operating costs are those costs associated with the day-to-day physical operation of housing projects and may include utilities (including internet), maintenance and repairs, marketing and leasing costs taxes and insurance, property management, office supplies and expenses, legal and accounting services, security and/or site monitors, cleaning fees, and housing incidentals (refrigerators/appliances, water heater, transportation, furnishings, food, hygiene products etc.). Operating costs may not include costs for behavioral health services; however, these can be covered under BHSS and other behavioral health funding sources. Operating costs may not include costs for housing transition navigation or tenancy sustaining services; however, the costs for these services are included as allowable expenditures in the “other housing supports” component of Housing Interventions (see Chapter 7, Section C.9.4 below). Counties opting to provide operating subsidies as a Housing Intervention service must develop policies and procedures that, at a minimum, address the types of expenses which may be covered with Housing Interventions.
C.9.3 Allowable Settings
The aim of Housing Interventions is to help individuals achieve permanent housing stability. To the maximum extent possible, counties should seek to place individuals in permanent housing settings.
However, Housing Interventions may also be used in connection with placement in interim settings for a limited time. For BHSA eligible individuals who have exhausted the Transitional Rent benefit, counties may use the BHSA Housing Interventions funding to provide an additional six months of subsidy for placement in an interim setting. For BHSA eligible individuals who are not eligible for Transitional Rent, 12 months of coverage in an interim setting may be provided. After the 6- or 12-month time limit has expired, Housing Interventions funds may only be used for placement in a permanent setting.
Housing Interventions funding will be permissible in the following settings:
Non-Time-Limited Permanent Settings:
Supportive housing
Apartments, including master-lease apartments
Single and multi-family homes
Housing in mobile home communities
Single room occupancy units
Accessory dwelling units, including Junior Accessory Dwelling Units
Tiny Homes[132]
Shared housing
Recovery/Sober Living housing, including recovery-oriented housing[133]
Assisted living (adult residential facilities, residential facilities for the elderly, and licensed board and care)
License-exempt room and board
Other settings identified under the Transitional Rent benefit
Time Limited Interim Settings:
Hotel and motel stays
Non-congregate interim housing models
Congregate settings that have only a small number of individuals per room and sufficient common space (not larger dormitory sleeping halls)[134] (does not include behavioral health residential treatment settings)
Recuperative Care
Short-Term Post-Hospitalization housing
Tiny homes, emergency sleeping cabins, emergency stabilization units
Peer respite
Other settings identified under the Transitional Rent benefit
Counties must ensure that individuals are voluntarily placed in the least restrictive, most community-integrated setting that can accommodate their physical and behavioral health needs.
Individuals should be placed in settings that reflect their preferences and goals, enables them to stay in their “home” communities and provides for community integration in accordance with all applicable federal and state law.
C.9.3.1 Permanent Supportive Housing
Permanent Supportive Housing (PSH) is a proven and cost-effective model that provides long-term housing coupled with intensive case management services linking individuals with medical, behavioral health, and other services such as income supports. Those supports can be referrals to community-based providers or delivered onsite, depending on the nature of the project or the tenants’ needs. When integrated with voluntary, flexible, intensive community-based services, PSH is an evidence-based practice that is nationally recognized as the standard solution for meeting the housing needs of people with serious mental illness. Basic tenets of PSH, including those enumerated in Housing First, include:
Permanent: Tenants may live in their homes as long as they meet the basic obligations of tenancy, such as paying rent.
Supportive: Tenants have access to the supportive services that they need and want to retain housing.
Housing: Tenants have a private or shared and secure place to make their home, just like other members of the community, with the same rights and responsibilities.
PSH programs may be administered through tenant-based rental subsidies, which may be used in the private rental market, or through site-based subsidies or vouchers (rental assistance), that are attached to particular units. PSH requires a rental contract or lease between the tenant/program participant and a property owner/landlord. The tenant may pay a portion of the rent (typically no more than 30 percent of the tenant’s adjusted monthly income) and the PSH program covers the remaining portion of rent to the owner/landlord/property.
County-led PSH rental subsidy programs should adopt policies that outline the parameters and procedures of the administration of the subsidies. Among those are definition of eligible participants, eligible units (i.e., compliance with rent reasonableness and housing quality standards), and rental contribution income calculation methodology. Counties are encouraged to adhere to the Department of Housing and Urban Development (HUD) standards for PSH rental calculations.
Leases are required, and those leases or other occupancy agreements shall comply with state and local laws and not impose additional barriers or behavioral standards not contained in standard lease agreements.
PSH is an effective model even for individuals with significant and complex behavioral health conditions; individuals with frequent and long-term hospitalizations, homelessness, and incarceration succeed in PSH with intensive supports, such as Assertive Community Treatment (ACT) or Intensive Case Management (ICM). An independent evaluation from 2020 using a randomized control trial in Santa Clara County, for example, found that PSH is associated with increases in housing placement, increases in housing retention, increases in outpatient mental health service utilization, and decreases in psychiatric-related emergency department utilization among individuals with the most acute needs. Counties are encouraged to assess the opportunity to leverage BHSA Housing Interventions with other programs providing capital funding for PSH units for BHSA eligible individuals, including Veterans, such as Homekey+, No Place Like Home (NPLH), and Community Care Expansion (CCE).
C.9.3.2 Shared Housing
Many communities have programs that use rental assistance for shared housing, which is when more than one person or household agrees to share a housing unit. Each person (or couple as they choose) must have their own bed and locked cabinet/bureau. In some cases, programs will offer private bedrooms. In all cases, participants must have access to common areas such as the kitchen, bathroom, and living room. Shared housing is an effective way to make housing more affordable, to maximize available housing stock, and to decrease isolation for people not used to living alone.
Typically, each household has its own lease or sublease, and shares expenses like utilities. Rent is split by the number of bedrooms, and the rent reasonableness standard is applied per tenant/household. The tenant’s contribution may be based on percent of income as described above.
Shared Housing is a subset of rental assistance, and counties opting to provide shared housing should develop policies and procedures with specific callouts for best practices for shared housing. Those practices include the following:
Participant choice is one of the hallmarks of success in shared housing programs. Participants should opt into shared housing and feel informed about the logistics and pros and cons of the arrangement as well as feel empowered in the creation of shared household rules and norms.
Roommate matching is key to success; some roommate matches may occur organically, through meetings at shelter or in other programs. Many providers use a roommate matching process, much like those used for college dorms or other roommate situations, to help participants define preferences. For example, individual preferences for roommates may include gender, pets, substance use rules, quiet hours, or cleanliness.
Roommate agreements can help support roommates in living in a shared space; and some programs will have peer or case management facilitation for this process and for dispute resolution.
C.9.3.3 Recovery Housing
Recovery housing is a housing intervention that is recognized by both Substance Abuse and Mental Health Services Administration (SAMHSA) and HUD as an important housing option for individuals with substance use disorders.[135] Recovery housing, also referred to as sober living or recovery residences, offers shared housing in a milieu that is supportive of recovery and that builds a sense of community and mutual support. Recovery housing, including recovery-oriented housing, can provide valuable support for those in outpatient treatment, leaving residential treatment, or others seeking to live in an alcohol and drug-free environment that supports recovery and wellness. The American Society of Addiction Medicine (ASAM) Criteria, Fourth Edition, includes recovery residences as a part of the continuum of care.
People who want to live in a recovery environment should have access to recovery housing; however, individuals who prefer low-barrier housing must not be limited to recovery housing. In other words, recovery housing should be an option but must never be the only option available to individuals in need of housing interventions.
Recovery housing should be designed to promote community, prosocial behaviors, and mutual support. Additionally, recovery housing providers must ensure the rights of privacy, dignity, and respect of residents and have policies in place that allow for all medications for addiction treatment approved by the FDA to treat substance use disorders. Other requirements include providing a lease or at minimum a participant agreement, supportive services for both relapse prevention and relapse support, and appropriate referrals for an individual who chooses not to stay or must leave. Recovery housing providers are encouraged to meet the National Association of Recovery Residences national standards for recovery housing.
Most recovery housing is transitional with people staying up to one year then moving to permanent housing once they have built their recovery capital and found supportive, affordable housing. There are different levels of recovery housing starting with varying staffing and services and requirements. Some recovery housing providers require participation in outpatient treatment. There is some recovery housing that is permanent housing with no maximum length of stay. There are also some recovery housing options designed for specific populations including transition age youth, families with children, LGBTQIA+ populations, and faith communities.
C.9.3.4. Assisted Living (Adult Residential Care Facilities, Residential Care Facilities for the Elderly, and Licensed Board and Care Facilities)
Housing Interventions may help to cover stays in Adult Residential Facilities, Residential Care Facilities for the Elderly, Board and Care facilities, and license-exempt room and board facilities. Such facilities provide 24/7 care to people who require it due to cognitive impairment or inability to perform activities of daily living (ADLs), along with room and board. These settings may be appropriate for some people experiencing homelessness who have serious behavioral health conditions, require assistance with ADLs, or have severe cognitive impairment.
Housing Interventions funding for these facility types is not time-limited. However, Title II of the Americans with Disabilities Act, as affirmed by the U.S. Supreme Court in Olmstead v. L.C. (1999), requires states to provide services to individuals with disabilities in the most integrated setting appropriate to their needs. This means that eligible individuals should only be placed in such settings where medically necessary and only for as long as medically necessary. Eligible individuals who are able to reside in PSH or other more independent settings should be transitioned as soon as possible.
C.9.3.5 Recuperative Care
Recuperative Care, also referred to as medical respite care, is short-term residential care for individuals who no longer require hospitalization, but still need to heal from an injury or illness (including behavioral health conditions) and whose condition would be exacerbated by an unstable living environment. An extended stay in a recovery care setting allows individuals to continue their recovery and receive post-discharge treatment while obtaining access to primary care, behavioral health services, case management and other supportive social services, such as transportation, food, and housing.
Recuperative Care is available as a Medi-Cal Community Support. If Recuperative Care can be covered by a Medi-Cal Managed Care Plan (MCP), the Medi-Cal service must be used before Housing Interventions. Housing Interventions may be used for the costs of room and board in Recuperative Care for BHSA eligible individuals not eligible to receive coverage of this service from their MCP. Behavioral health services provided during Recuperative Care cannot be funded through Housing Interventions.
C.9.3.6 Short-Term Post-Hospitalization Housing
Short-Term Post-Hospitalization Housing provides BHSA eligible individuals who do not have a residence and who have high medical or behavioral health needs with the opportunity to continue their medical/psychiatric/substance use disorder recovery immediately after exiting an inpatient facility (either acute or psychiatric or Chemical Dependency Recovery hospital, or psychiatric health facility), residential substance use disorder treatment or recovery facility, residential mental health treatment facility, correctional facility, nursing facility, or Recuperative Care and avoid further utilization of these services.
This setting must make available ongoing supports necessary for recuperation and recovery such as gaining (or regaining) the ability to perform activities of daily living, receiving necessary medical/psychiatric/substance use disorder care, utilizing case management, and accessing other housing supports. This setting may include an individual or shared interim housing setting, where residents receive the services described above.
Short-Term Post-Hospitalization Housing is available as a Medi-Cal Community Support. If Short-Term Post-Hospitalization Housing can be covered by an MCP, the Medi-Cal service must be used before Housing Interventions. Housing Interventions funds may be used for the costs of room and board in Short-Term Post-Hospitalization Housing for BHSA eligible individuals not eligible to receive coverage of the service from their MCP. Behavioral health services provided during Short-Term Post-Hospitalization Housing cannot be funded through Housing Interventions.
C.9.4 Other Housing Supports
Counties may provide other housing supports as identified by DHCS in this guide, in addition to the housing interventions specifically identified in W&I Code section 5830, subdivision (b), including, but not limited to, those listed in the Medi-Cal Community Supports Policy Guide.[136] Pursuant to this authority, counties may provide under the category of ”other housing supports”: (1) Landlord Outreach and Mitigation Funds, (2) Participant Assistance Funds, (3) Housing Transition Navigation Services and Housing Tenancy and Sustaining Services and (4) Outreach and Engagement (up to 7 percent). However, as described throughout this section, BHSA funds may not be used for Medi-Cal services that can be covered and funded through the individual’s Medi-Cal managed care plan (MCP). In other words, BHSA funds can only be used for Community Supports if the MCP has chosen not to administer the service, the individual is not eligible for the service, or the individual’s needs exceed service limitations and as such the service cannot be covered as a Community Support.
C.9.4.1 Landlord Outreach and Mitigation Funds
Landlord Outreach and Mitigation Funds may be used to support outreach to, and engagement of, landlords and property owners, which may include the development of presentations, outreach materials, campaigns, and support to help properties meet the requirements of Housing Interventions. Landlord Outreach and Mitigation Funds may also be used by counties to encourage and incentivize property owners to rent to eligible individuals. Additionally, counties may establish a mitigation fund to offset any damages caused by a Housing Interventions participant and/or for use in connection with potential or actual evictions as further described below.
Counties opting to provide Landlord Outreach and Mitigation Funds as part of their Housing Interventions must develop policies and procedures that, at a minimum, address the following:
Enumerate the types of landlord outreach costs that Housing Interventions will cover and the maximum allowable reimbursement, examples include:
Development of outreach materials (e.g., graphic design).
Costs associated with advertising and campaigns focused on landlord recruitment, including networking events (e.g., attending/presenting at local landlord associations).
Landlord incentives (e.g., one-time incentives, signing bonus, referral bonus).
Holding fees (short term costs to hold a vacant unit before a tenant moves in).
Enumerate the types of landlord mitigation costs that Housing Interventions will cover and the maximum allowable reimbursement, examples include:
Damage reimbursement outside of usual wear and tear.
Unit hold related costs and vacancy payment (if tenant leaves early) or if PBH unit is vacant for a specified number of days after sufficient marketing.
Eviction prevention costs which may include financial assistance, back-rent, mediation, tenant education, legal costs and connection to resources (if necessary for someone to maintain their housing or be relocated).
Identify protocols for approving allowable costs and mechanisms for documenting costs.
Identify processes for the prevention of fraud, waste, and abuse
Identify any overlap with other community funds and create procedures to avoid duplication.
These policies and procedures are not subject to review and approval by DHCS but must be provided to DHCS upon request.
C.9.4.2 Participant Assistance Funds
Counties may use Housing Interventions to establish Participant Assistance Funds that seek to remove barriers to housing and support people in meeting their immediate housing needs. Any support provided should be based on individualized assessment of needs. Examples of services and activities to be covered under a Participant Assistance Fund may include, but would not be limited to:
Costs associated with obtaining government-issued identification and other vital documents
Housing application fees
Fees for credit reports
Security deposits
Utility deposits
Storage fees
Pet deposits and other pet fees
Move-in costs, including costs associated with establishing a household such as:
Transportation
Food
Hygiene products
Moderate furnishings (including but not limited to items such as a bed, tables and chairs, cleaning tools, and other supplies that people need to settle into housing)
Rent and utility arrears
The Medi-Cal Housing Deposits Community Support covers many of the expenses identified above.[137] Housing Interventions may not be used to cover expenses that an individual’s MCP would cover under the Housing Deposits Community Support (assuming the individual is enrolled in an MCP and eligible for Housing Deposits). However, Housing Interventions may be used for expenses not covered under Medi-Cal Housing Deposits, such as pantry stocking. For individuals not eligible for Housing Deposits or who have exhausted the Housing Deposits covered by their MCP, Housing Interventions may be used for the complete list of expenses covered by the county’s Housing Interventions under its Participant Assistance Fund.[138]
Counties opting to provide Participant Assistance Funds as a Housing Interventions service must develop policies and procedures that, at a minimum, address the following:
Enumerate the types of costs that may be covered.
Identify protocols for approving allowable costs and mechanisms for documenting costs.
Identify processes for the prevention of fraud, waste, and abuse.
Identify any overlap with other community resources (for example, the Housing Deposits Community Support or other rental assistance deposit funds) and create procedures to avoid duplication of services.
These policies and procedures are not subject to review and approval by DHCS but must be provided to DHCS upon request.
C.9.4.3 Housing Transition Navigation Services and Housing Tenancy Sustaining Services
Counties may fund Housing Transition Navigation Services and Housing Tenancy Sustaining Services for individuals not eligible for these services through a Medi-Cal MCP. Counties using Housing Interventions to fund Housing Transition Navigation Services and Housing Tenancy Sustaining Services shall refer to the Community Supports policy guide for a list of allowable activities but are not subject to the eligibility, restrictions/limitations, or licensing/allowable provider requirements set forth in the Medi-Cal guidance or any other requirements established for Medi-Cal, if not additionally specified as applicable to BHSA Housing Interventions. Counties may also become contracted Community Supports providers which enables counties to provide Housing Transition Navigation Services and Housing Tenancy Sustaining Services to individuals enrolled in Medi-Cal.
C.9.4.4 Outreach and Engagement
Outreach and engagement activities may only represent up to 7 percent of the Housing Interventions funding allocation in accordance with the transfer guidelines in C.6 Transfers and Exemptions. Outreach and engagement activities should be tracked and entered into HMIS to inform key metrics such as the number of individuals contacted, the percentage of individuals who received housing assistance, the housing retention rate, the number of new community partnerships formed, and qualitative feedback from participants and community partners.
In alignment with the engagement activities identified as allowable under the United States Department of Housing and Urban Development Emergency Solutions Grant funding, engagement activities may include the activities necessary to locate, identify, and build relationships with individuals or families living in unsheltered settings for the purpose of providing immediate support, intervention, and connections with homeless assistance programs or mainstream social services and housing programs. Outreach and engagement activities shall not duplicate services provided by Medi-Cal MCPs per W&I Code 5830(c)(2).
Activities may include but not limited to:
Building relationships either through one-on-one engagement or by conducting regularly-scheduled broad outreach in high-need areas in conjunction with community partners.
The purchase and distribution of items like food, hygiene products, clothing, blankets, and water to provide immediate support and foster future service engagement.
Providing immediate, onsite direct navigation to housing resources.
Coordinating behavioral health service and housing resources for unsheltered individuals in collaboration with other outreach and engagement efforts.
Travel by outreach workers, social workers, medical professionals, or other service providers during the provision of eligible street outreach services. Also includes the costs of transporting unsheltered people to emergency shelters or other service facilities.
Harm reduction activities and the distribution of harm reduction supplies.
C.9.5 Other Housing Interventions Requirements and Policies
This section discusses other requirements and policies that apply to Housing Interventions services.
C.9.5.1 Housing First
Housing Interventions must be operated in compliance with the core components of Housing First and “may include recovery housing.”[139],[140] Housing First is defined in statute[141] as “the evidence-based model that uses housing as a tool, rather than a reward, for recovery and that centers on providing or connecting homeless people to permanent housing as quickly as possible.”
Consistent with the national Housing First model and W&I Code section 8255, subdivision (b), abstinence from alcohol or other substances cannot be a requirement or prerequisite for Housing Interventions services. Additionally, the use of alcohol or other substances in and of itself cannot be grounds for eviction and Housing Interventions services are informed by a harm-reduction philosophy that recognizes drug and alcohol use and substance use disorder (SUD) as a part of tenants’ lives, where tenants are engaged in nonjudgmental communication regarding drug and alcohol use; and where tenants are offered education regarding how to avoid risky behaviors and engage in safer practices, as well as connected to evidence-based treatment if the individual so chooses. However, Housing Interventions may be used to support recovery housing and sober living environments for individuals who request them. Counties must ensure that in their implementation of Housing Interventions, neither they, nor entities that receive the BHSA Housing Interventions dollars, discriminate against or deny access to housing for individuals who are utilizing medications for addiction treatment or other authorized medications.
In alignment with the California Interagency Council on Homelessness “Guide to California’s Housing First Law” Housing First law applies to both permanent and interim housing settings. While the requirement of a lease may not be applicable to interim settings, they must use Housing First components and principles for screening and selecting participants and in providing services and other engagement with participants.
The Department of Housing and Urban Development (HUD) provides valuable resources on Housing First that a county may look to for guidance on how to apply Housing First principles.
C.9.5.2 Family Housing
All Housing Interventions, as appropriate, must be available to support Family Housing. As defined by HUD, “Family” includes, but is not limited to, regardless of marital status, actual or perceived sexual orientation, or gender identity, any group of persons presenting for assistance together with or without children and irrespective of age, relationship, or whether or not a member of the household has a disability. A child who is temporarily away from the home because of placement in foster care is considered a member of the family.
Family Housing means housing that prioritizes not separating individuals meeting the definition of family. Family housing includes housing that accommodates the family caregiver of a BHSA eligible child, adult, older adult, or a person living with a disability.
Family housing for children and youth considerations include:
Design, location, and environmental impacts of the housing interventions provided to the family. Dedicated space for children and youth, including green space, open space, secure play areas and courtyards, as well as indoor space in which children may play and learn are some examples.
Access to public transportation, walkable neighborhoods or bike path access benefit children and youth and their parents.
Where a child is eligible for Housing Interventions, the family is eligible for Housing Interventions services, even if the parent or guardian is not independently eligible, provided that the parent or guardian lives with the child. Emancipated minors are eligible to receive Housing Interventions services directly. In the reverse situation (parent or guardian is eligible but child is not), the housing provided should accommodate the whole family living together (including children).
Family housing for adults and older adults considerations include:
Accommodations that meet the needs of the BHSA eligible individual (e.g., wheelchair ramps) as well as proximity to amenities such as community spaces, public transportation, and clinical care.
C.9.5.3 Habitability Standards
Housing Interventions may only be used in connection with housing settings that meet minimum standards for habitability. Effective October 1, 2025, all units subject to HUD quality requirements will be required to meet a new set of standards titled the National Standards for the Physical Inspection of Real Estate (NSPIRE).[142] This will replace the HUD Housing Quality Standards. While DHCS expects counties to seek to fund settings that meet NSPIRE standards whenever possible, an attestation that the housing is habitable as defined by state law[143] and meets applicable state and local building standards will meet the minimum requirement for Housing Interventions funding. These standards will be implemented in alignment with the standards identified under Transitional Rent. Inspection costs are an allowable expense under Housing Interventions.
C.9.5.4 Minimum Quality Standards
Counties must ensure that all settings for which Housing Interventions are expended meet minimum quality standards. Many of the settings eligible for coverage serve populations with significant needs but are unlicensed and have been found to be of widely varying quality. This would include, for example, recovery residences and sober living environments as well as license-exempt room and board facilities. These standards will be implemented in alignment with the standards identified under Transitional Rent.
C.9.5.5 Homeless Management Information System Requirements
Counties are required to operate Housing Interventions in accordance with the Homeless Management Information System (HMIS) reporting requirements.[144]
Counties are required to enter into the local HMIS the Universal Data Elements (Items 3.01-3.917) and the Common Data Elements (Items 4.02-4.20 and Item W5 of the Individual Federal Partner Program Elements) as defined by the HUD HMIS Data Standards for the individuals and families served, as required by W&I Code section 8256, subdivision (d)(8).
Every Continuum of Care (CoC) must designate an HMIS lead entity. The HMIS lead is responsible for administering, implementing, and managing the HMIS database as well as training and supporting HMIS users. Counties should work closely with the HMIS lead in their community to complete program setup and ensure data quality is meeting expectations. This list of CoC leads in California includes the HMIS leads for most communities. Coordination with the local Coordinated Entry System (CES) is strongly encouraged but counties are not required to route referrals for housing interventions through the CES.
C.10 Capital Development Projects
Increasing the supply of PSH and other affordable housing is critical to addressing California’s homelessness crisis. Housing Interventions may include capital development projects that increase the supply of PSH, or affordable units that provide long-term housing stability and supportive services to eligible individuals and their families. For individuals who meet the eligibility and priority populations criteria, maintaining residential stability without greater assistance can be difficult. Many of these individuals and families are challenged by health conditions, social isolation, and deep poverty, and face significant barriers to both work and housing. However, studies have shown that even high-risk individuals can be successfully housed if PSH is available.[145]
Counties will be required to detail their proposed capital development projects in their Integrated Plans (IPs) and annual updates (AUs). The DHCS encourages counties to employ and include in their IP innovative practices to develop permanent supportive housing and other affordable housing in the most efficient, timely and cost-effective manner available to the county. This section provides guidance regarding the requirements for capital development projects.
C.10.1 Capital Development Project Funding
Counties may use no more than 25 percent of their Housing Interventions on capital development projects.[146] Counties may use capital development project funds to fully fund a capital development project or to fill gaps in funding within a larger development that includes a set number of units dedicated to PSH for BHSA eligible individuals and their families.
Key elements of capital development funding:
Counties may accrue their capital development project funding for multiple years to cover the cost of a project provided that the county complies with the rules regarding reversion. See Chapter 6 for more details about the reversion of funding to the state.
Generally, there is no single funding source for PSH developments. Consequently, counties and project developers may also combine funding from other federal, state, and local sources to develop properties that include PSH units provided that the project meets the requirements for capital development projects. Counties are encouraged to align their capital development funding requirements with other local, state and federal programs that will help braid requirements and funding from multiple programs – this practice can reduce administrative burden and related costs for counties and housing sponsors.
The maximum amount of capital development funds that a county may use to fund the construction and/or rehabilitation of housing units under this program is $450,000 per unit.
C.10.2 Eligibility and Access Requirements
Counties may use capital development funding for the construction and/or rehabilitation of housing units provided that the projects meet the following eligibility and access requirements:
The housing units must be made available to individuals and families who meet the eligibility and priority populations criteria as defined in Chapter 7, Section C.4.1 “Eligible Populations”.
Access to housing units may not be limited to individuals enrolled in FSP or to those enrolled in Medi-Cal.
Capital development projects may not discriminate against or deny access to housing for individuals who are utilizing medications for addiction treatment or other authorized medications.
Capital development projects must comply with the core components of Housing First.
C.10.3 Capital Development Project Requirements
The following additional requirements apply to projects receiving capital development project funding:
The housing units constructed and/or rehabilitated must be affordable and satisfy the definition of “supportive housing.” As provided in California Government Code section 65582, subdivision (g), “supportive housing” means “housing with no limit on length of stay, that is occupied by the target population, and that is linked to onsite or offsite services that assist the supportive housing resident in retaining the housing, improving their health status, and maximizing their ability to live and, when possible, work in the community.”
The housing units must be available for Eligible individuals and their families within a reasonable timeframe that is consistent with each county’s approved Integrated Plan.
To constitute a “use by right” the project must meet all of the requirements under W&I Code section 5831, subdivision (a)(1).
The project must comply with any other requirements specified by DHCS for purposes of administering county capital development programs.
Funding for capital development projects are subject to the three and five-year reversion periods.
C.10.4 Exemption from the Low Rent Housing Project Requirements
Capital development projects are exempt from the low rent housing project requirements in the California Constitution and related statutes, which require voter approval of such projects. While there are multiple criteria for an exemption, BHSA projects are identified as one of the exemption criteria. Specifically, if the capital development project consists of the “acquisition, rehabilitation, reconstruction, alterations work or new construction or any combination” of these with respect to lodging facilities or dwelling units funded using moneys from the Behavioral Health Services Fund (BHSF), the project is exempt from the low rent housing project requirements in Section 1 of Article XXXIV of the California Constitution.[147]
C.10.5 Exemptions Available to Projects that Meet “Use by Right” Requirements
To allow for the efficient use of capital development project funds and the timely construction and/or rehabilitation of PSH units, W&I Code section 5831 limits the application of permitting, land use requirements and environmental requirements to capital development projects that satisfy the “use by right” requirements and meet specified criteria. These rules are intended to prevent capital development projects from being delayed by time-consuming subjective and discretionary approval processes and related litigation.
As further specified in the Appendix, the BHSA limits local governmental review of such projects to the application of objective zoning, subdivision, and design standards which must be applied within strictly limited timeframes. It also exempts BHSA-funded projects that meet the “use by right” requirements from the California Environmental Quality Act.
[1] W&I Code, § 5892 subdivision (a)(3)(A)
[2] According to W&I Code, § 5892 subdivision (a)(3)(i), Children’s System of Care services and requirements are described in Part 4, commencing with W&I Code, § 5850. Adult and Older Adult System of Care services and requirements are described in Part 3, commencing with W&I Code, § 5800. These services do not include Housing Interventions or Full Service Partnership services.
[3] W&I Code, § 5892 subdivision (k)(4)
[4] Department of Health Care Services, BHIN 22-026: Drug Medi-Cal (DMC), Drug Medi-Cal Organized Delivery System (DMC-ODS) and Specialty Mental Health Services (SMHS) Peer Support Services: “Peer Support Services include the following service components: […] Engagement means Peer Support Specialist led activities and coaching to encourage and support beneficiaries to participate in behavioral health treatment. Engagement may include supporting beneficiaries in their transition between levels of care and supporting beneficiaries in developing their own recovery goals and processes.”
[5] https://www.dhcs.ca.gov/CalAIM/Pages/Opt-in-to-BH-CONNECT.aspx
[6] W&I Code § 5892, subdivision (k)(5)
[7] “Regional Partnership” is defined as a group of county-approved individuals and/or organizations within geographic proximity that acts as an employment and education resource for the county behavioral health delivery system. The group may include educational and employment service entities, individuals and/or entities within the county behavioral health delivery system, and individuals and/or entities that have an interest in the county behavioral health delivery system, such as county staff, mental health or substance use treatment service providers, individuals receiving services, and their family members.
[8] W&I Code, § 5892 subdivision (a)(4)(A)
[9] W&I Code, § 5840 subdivision (a)(1), W&I Code, § 5892 subdivision (a)(3)(A)(ii)
[10] W&I Code 5892(a)(3)(B), W&I Code, § 5892 subdivision (a)(3)(B)(ii)
[11] W&I Code, § 5892 subdivision (a)(4)(A)
[12] W&I Code § 5840 subdivision (d)
[13] Underserved cultural populations means those who are unlikely to seek help from providers of traditional mental health and substance use disorder services because of stigma, lack of knowledge, or other barriers, including members of ethnically and racially diverse communities, members of the 2S/LGBTQ+ communities, victims of domestic violence and sexual abuse, and veterans, across their lifespans.
[14] W&I Code, § 5840.6, subdivision (f)(1), W&I Code, § 5840.6, subdivision (f)(2).
[15] W&I Code, § 5840.6, subdivision (f)
[16] Overview of the Institute of Medicine’s Continuum of Care is detailed by SAMHSA’s Strategic Prevention Technical Assistance Center
[18] W&I Code § 5840; W&I Code § 5892
[19] W&I Code § 5840.7, subdivision (b)
[20] W&I Code § 5840.7, subdivision (b)(1)(B)(i)-(ii)
[21] W&I Code § 5840.7, subdivision (b)(2)
[22] W&I Code § 5840.6, subdivision (c)
[23] W&I Code § 5840, subdivision (b)
[24] W&I Code, § 5840 subdivision (b)(1)
[25] W&I Code, § 5892 subdivision (d)
[26] W&I Code, § 5840.6 subdivision (g)
[27] W&I Code, § 5840.6 subdivision (e)
[28] W&I Code, § 5840.6 subdivision (g)
[29] W&I Code § 5840.6, subdivision (e)
[30] W&I Code § 5840, subdivision (b)(2)(A)
[31] W&I Code, § 5840 subdivision (b)(2)(B)
[32] W&I Code, § 5840 subdivision (b)(3)
[33] Supports under the mental health and substance use disorder services and supports component are separate and distinct from “housing supports” provided within Housing Interventions.
[34] W&I Code, § 5840 subdivision (b)(3)(C)
[35] W&I Code, § 5840 subdivision (c)(4)
[36] The DHCS Trauma Informed Care webpage includes the ACEs Aware screening tool and other resources.
[38] W&I Code § 5835, subdivision (b)(2)
[39] Nossel I., Wall, M., et. al. (2018) “Results of a Coordinated Specialty Care Program for Early Psychosis and Predictors of Outcomes.” Psychiatry Serv. 1;69(8):863-870.
[40] Breitborde, N., Bell, E., et. al. (2023).“The Early Psychosis Intervention Center (EPICENTER): development and six-month outcomes of an American first-episode psychosis clinical service.” BMC Psychiatry. 15(266).
[41] Kane, M., Delbert, G., et.al. (2015). “Comprehensive Versus Usual Community Care for First-Episode Psychosis: 2-Year Outcomes from the NIMH RAISE Early Treatment Program.” American Journal of Psychiatry. 173(4).
[42] Heinssen, R., Goldstein, A., and Azrin, S. (2023). “Evidence-Based Treatments for First Episode Psychosis: Components of Coordinated Specialty Care.”
[43] A city receiving BHSA funding can meet this requirement if the county will be providing CSC for FEP and/or opting into the bundled benefit.
[44] Consistent with the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) mandate, counties are required to provide CSC for FEP to Medi-Cal members under the age of 21 if the service is clinically appropriate.
[45] APL 24-007 Implementation of Senate Bill 855 Regulation, Mental Health and Substance Use Disorder Coverage
[46] W&I Code § 5891, subdivision (a)(3)(A)
[47] W&I Code § 5840, subdivision (c)(1)
[48] W&I Code § 5840, subdivision (c)(5)
[49] DHCS. Behavioral Health Community-Based Organized Networks of Equitable Care and Treatment (BH-CONNECT) Initiative.
[50] DHCS. “Evidence-Based Practices and Community-Defined Evidence Practices Grant Program.
[52] Blueprints for Healthy Youth Development
[53] The Athena Forum. Excellence in Prevention Strategy List.
[54] Psychology Applied Research Center of Loyola Marymount University, The California Reducing Disparities Project Phase 2 Statewide Evaluation / California Pan-Ethnic Health Network. California Reducing Disparities Project Strategic Plan to Reduce Mental Health Disparities: Executive Summary.
[55] SAMHSA. Evidence-Based Practices Resource Center.
[56] University of Cincinnati Corrections Institute. Cognitive-Behavioral Intervention - Substance Use (CBI- SU) curriculum.
[57] California Department of Social Services’ Office of Child Abuse Prevention. Scientific Rating Scale.
[58] Los Angeles County Department of Mental Health. Prevention and Early Intervention Plan.
[59] MHSOAC. “Report to the Legislature on Full Service Partnerships”. January 25, 2023
[60] Ibid.
[61] MHSOAC. “Transformational Change: Full Service Partnerships. Third Sector Report Summary”. May 23, 2024.
[62] All of these services are covered Medi-Cal services with dedicated bundled rates (ICM is covered under Medi-Cal but does not have a dedicated bundled rate). DHCS encourages counties to opt-in to provide these services under Medi-Cal. When counties opt-in to provide these services under Medi-Cal, they will receive the bundled rate when providing services to Medi-Cal members and may use FSP funding for the non-federal share.
[63] Providers are responsible for attempting to engage FSP-eligible individuals to ensure they are adequately supported in their recovery. If the team attempts to engage an FSP-eligible individual repeatedly for several months and are unable to engage them, the team should meet and discuss whether that individual should be moved to a lower level of care or disenrolled so that another FSP-eligible individual is able to receive services.
[64] Housing Interventions provided to FSP clients must be funded through the Housing Interventions component. All Medi-Cal billable services must be billed to Medi-Cal pursuant to W&I Code § 5891(a)(1)(G)(2).
[65] Counties who are Enhanced Care Management (ECM) Providers can deliver ECM to individuals receiving FSP and counties have discretion to prioritize FSP program slots for individuals not eligible for ECM Policy Guide for additional information.
[66] DHCS has discretion to define additional evidence-based services, treatment models, and community defined practices and may do so in future iterations of the policy manual. The addition of evidence-based services, treatment models, and community defined practices will include stakeholder consultation.
[67] FSP ICM is a required service pursuant to W&I Code § 5887(e) directing DHCS to establish FSP levels of care and is explained later in the chapter.
[68] County FSP programs are expected to adhere to the service planning process outlined in W&I Code sections 5806 and 5868 and do not require documentation in a “standalone” treatment plan or service plan.
[69] W&I Code § 5887, subdivision (d)
[70] Counties with populations under 200,000 that have not achieved fidelity implementation of one or more EBPs in advance of June 30, 2029, will have an opportunity to seek an exemption from ACT and FACT, or a fidelity exemption for IPS and HFW, for the 2029 - 2032 IP, and may use findings from the COE review or other supporting data to support that request.
[71] Counties are still expected to meet fidelity requirements for HFW in accordance with providing these services through Medi-Cal under EPSDT.
[72] Strategies to build co-occurring capabilities are an allowable use of FSP funding.
[73] Please see BHIN 23-054 for DHCS’s existing MAT policy and definition of an “effective referral.”
[74] W&I § 5892, subdivision (k)(7)
[75] van Vugt MD, Kroon H, Delespaul PA, Mulder CL. Assertive community treatment and associations with substance abuse problems. Community Ment Health J. 2014 May;50(4):460-5. doi: 10.1007/s10597-013-9626-2. Epub 2013 Jun 15. PMID: 23771775.
[76] Marshall M, Lockwood A. Assertive community treatment for people with severe mental disorders. Cochrane Database Syst Rev. 2000;(2):CD001089. doi: 10.1002/14651858.CD001089. Update in: Cochrane Database Syst Rev. 2011 Apr 13;(4):CD001089. doi: 10.1002/14651858.CD001089.pub2. PMID: 10796415.
[77] Penzenstadler L, Soares C, Anci E, Molodynski A, Khazaal Y. Effect of Assertive Community Treatment for Patients with Substance Use Disorder: A Systematic Review. Eur Addict Res. 2019;25(2):56-67. doi: 10.1159/000496742. Epub 2019 Jan 30. PMID: 30699412.
[78] Aagaard J, Tuszewski B, Kølbæk P. Does Assertive Community Treatment Reduce the Use of Compulsory Admissions? Arch Psychiatr Nurs. 2017 Dec;31(6):641-646. doi: 10.1016/j.apnu.2017.07.008. Epub 2017 Aug 10. PMID: 29179833.
[79] Burns T, Catty J, Dash M, Roberts C, Lockwood A, Marshall M. Use of intensive case management to reduce time in hospital in people with severe mental illness: systematic review and meta-regression. BMJ. 2007 Aug 18;335(7615):336. doi: 10.1136/bmj.39251.599259.55. Epub 2007 Jul 13. PMID: 17631513; PMCID: PMC1949434.
[80] W&I Code § 5891(a)((1)(G)(2)
[81] For Medi-Cal members, peer support specialists and Community Health Workers (CHWs) may also provide covered outreach and engagement services, as appropriate and consistent with Medi-Cal guidance.
[82] ACT is a stand-alone high-intensity mental health service delivery model and cannot be provided concurrently with FSP Intensive Services or HFW.
[83] Consistent with the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) mandate, counties are required to provide ACT to Medi-Cal members under the age of 21 if the service is clinically appropriate.
[84] Dieterich M, Irving CB, Bergman H, Khokhar MA, Park B, Marshall M. Intensive case management for severe mental illness. Cochrane Database of Systematic Reviews. 2017.
[85] Hangan C. Introduction of an intensive case management style of delivery for a new mental health service. Int J Ment Health Nurs. 2006.
[86] Guarino, K. Step by Step: A Comprehensive Approach to Case Management. 2011.
[87] Dieterich M, Irving CB, Bergman H, Khokhar MA, Park B, Marshall M. Intensive case management for severe mental illness. Cochrane Database of Systematic Reviews. 2017.
[88] Schaedle, R.W., Epstein, I. Specifying Intensive Case Management: A Multiple Perspective Approach. [89] Meyer, P., and Morrissey, J. A Comparison of Assertive Community Treatment and Intensive Case Management for Patients in Rural Areas. Psychiatric Services. 2007.
[90] Individuals with a primary diagnosis of intellectual/developmental disabilities (I/DD) are not appropriate for FSP Intensive Services.
[91] Counties are permitted but not required to mandate prior authorization or equivalent process.
[92] Additional services may be provided on an as needed basis.
[93] DHCS is not requiring an “on call” model of crisis intervention for FSP ICM participants.
[94] For Medi-Cal members, peer support specialists and CHWs may also provide covered outreach and engagement services, as appropriate and consistent with Medi-Cal guidance.
[95] National Wraparound Initiative, Portland State University
[96] Bruns et al. The Evidence Base and Wraparound. (2004)
[97] HFW is a stand-alone high-intensity mental health service delivery model and cannot be provided concurrently with ACT or FSP Intensive Services.
[98] Forthcoming Medi-Cal guidance will focus on billing Medi-Cal for HFW services, including meeting fidelity and other requirements. Find additional details about using BHSA funds for HFW services in the “Aligning HFW in FSP with Medi-Cal” section of this manual.
[99] IPS Employment Center, “IPS Introductory PowerPoint,” July 2021.
[100] IPS Employment Center, “Evidence for the Effectiveness of Individual Placement and Support Model of Supported Employment,” July 2022.
[101] Marsden J, Anders P, Shaw C, Amasiatu C, Collate W, Eastwood B, Horgan P, Khetani M, Knight J, Knight S, Melaugh A, Clark H, Stannard J. Superiority and cost-effectiveness of Individual Placement and Support versus standard employment support for people with alcohol and drug dependence: a pragmatic, parallel-group, open-label, multicenter, randomized, controlled, phase 3 trial. EClinicalMedicine. 2024 Jan 18;68:102400. doi: 10.1016/j.eclinm.2023.102400. PMID: 38299044; PMCID: PMC10828604.
[102] IPS Employment Center, 2024
[103] IPS Fidelity Scale, 2008
[104] Consistent with the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) mandate, counties are required to provide Supported Employment to Medi-Cal members under the age of 21 if the service is clinically appropriate.
[105] Los Angeles County. “Reaching the 95% Initiative.”
[106] City and County of San Francisco. “Street Overdose Response Team.”
[107] West Virginia Office of Drug Control Policy. “Programs: Quick Response Teams (QRT).”
[108] New Jersey Division of Mental Health and Addiction Services (DMHAS). “Opioid Overdose Recovery Program.”
[109] City of Portland, Oregon. “Community Health Asses and Treat (CHAT) Medication for Opioid Use Disorder (MOUD) and Overdose Response Team (ORT) Pilot Programs.”
[110] The “Three-Day Rule” (21 Code of Federal Regulations (CFR) § 1306.07(b)) allows prescribers unaffiliated with an NTP to administer methadone to a person “for the purpose of relieving acute withdrawal symptoms when necessary while arrangements are being made for referral for treatment. Not more than one day's medication may be administered to the person or for the person's use at one time. Such emergency treatment may be carried out for not more than three days and may not be renewed or extended.”
[111] California Department of Health Care Services. “All Plan Letter (APL) 24-001.” January 12, 2024. APL 24-001 provides more information and the different contracting options MCPs can take with street medicine providers, through direct contracting to serve as primary care and/or enhanced care management (ECM) providers, or as referring or treating contracted providers.
[113] Please refer to DHCS BHIN 24-005: “Mobile Narcotic Treatment Programs” for more detail regarding mobile NTP licensing.
[114] California Department of Public Health. “Syringe Services Programs in California: An Overview.”
[115] California Department of Health Care Services. “Medication Unit Application Overview.”
[116] Many SUD services in California, including all services covered through Drug Medi-Cal and the Drug Medi-Cal Organized Delivery System, are currently organized and delivered consistent with the American Society of Addiction Medicine (ASAM) criteria and corresponding levels of care. DHCS does not plan to define SUD FSP levels of care that deviate from these industry standard guidelines.
[118] Pursuant to W&I Code § 5891.5, subdivision (a)(2), the provision of Housing Interventions to individuals with a substance use disorder (SUD) is optional for counties in alignment with the requirements in Section 5963.02(b)(2) . However, when Housing Interventions are provided to an individual living with a SUD, all housing intervention requirements in W&I Code § 5830 must be met.
[119] W&I Code § 5892, subdivision (a)(1)(A)(ii).
[120] Unsheltered Homeless and Homeless Encampments in 2019
[121] W&I Code § 5892, subdivision (d)
[122] W&I Code § 5892, subdivision (c).
[123] W&I Code § 5892, subsections (a)(1)(B)-(C)
[124] W&I Code § 5830, subdivision (c)(2).
[125] As of September 6, 2024, 100 percent of MCPs cover the Housing Trio and 92 percent cover Recuperative Care and Short-Term Post-Hospitalization Housing. An additional six Medi-Cal managed care plans will offer Recuperative Care and Short-Term Post-Hospitalization Housing by 1/1/25. On 1/1/25, MCPs will have the option to cover Transitional Rent and on 1/1/26, coverage will be mandatory.
[126] DHCS Medi-Cal Community Supports Policy Guide. July 2023.
[127] DHCS CalAIM Community Supports – Managed Care Plan Elections. Updated July 2024.
[128] Coverage depicted as of date of publication – please refer to website for current status.
[129] DHCS Transitional Rent Concept Paper. August 2024.
[130] Fair Market Rent includes Small Area Fair Market Rent or up to 120% Fair Market Rent or Small Area Fair Market Rent.
[131] Time-limited interim settings must not require tenants to pay rent.
[132] Tiny homes would only be considered permanent if the settings have the hallmarks of a permanent setting such as requiring a lease, require payment of rent, has reasonable and ease of access to private bathrooms, kitchen areas, and utilities. Additionally, the settings must not have restrictive rules pertaining to curfews or having guests and has sufficient infrastructure to function as a permanent site.
[133] Single Room Occupancy and recovery housing can be interim or permanent. If interim, Housing Interventions is limited to 6 months for those who have exhausted Transitional Rent or 12 months for those who are not eligible for Transitional Rent. Please see Appendix B
[134] Congregate settings do not include behavioral health residential treatment settings. Housing Interventions may not be used to cover room & board in residential treatment settings.
[135] Substance Abuse and Mental Health Services Administration. Best Practices for Recovery Housing. Publication No. PEP23-10-00-002. Rockville, MD: Office of Recovery, Substance Abuse and Mental Health Services Administration, 2023.
[136] W&I Code § 5830, subdivision (b)(1)(F).
[137] See DHCS Medi-Cal Community Supports Policy Guide.
[138] For example, if an MCP covers the costs of Housing Deposits up to $8,000 and the individual has additional needs related to securing or establishing a home that cannot be met under this amount, additional expenses could be paid by Housing Interventions component. If the individual must pay fees or needs items not covered by the MCP, those too could be covered by Housing Interventions component.
[139] W&I Code § 8255, subdivision (b).
[140] W&I Code § 5830, subdivision (a)(5).
[141] W&I Code §§ 8255, subdivisions (d)(1)-(2)(A).
[143] See, e.g., California Civil Code §§ 1941, 1941.1, 1941.3.
[144] W&I Code § 8256, subdivision (d)(3)(A).
[145] Study finds Permanent Supportive Housing is effective for highest risk chronically homeless people.
[146] W&I Code § 5892, subdivision (a)(1)(A)(iii).
[147] W&I Code § 5830, subdivision (e)(8).
