3. County Integrated Plan
A. Purpose of the Integrated Plan
The Behavioral Health Services Act (BHSA) requires counties[1] to submit three-year Integrated Plans (IPs) for Behavioral Health Services and Outcomes. Whereas the Three-Year Program and Expenditure Plan required under the Mental Health Services Act (MHSA) focused exclusively on MHSA dollars, the BHSA establishes the IP to serve as a three-year prospective global spending plan that describes how county behavioral health departments plan to use all available behavioral health funding, including BHSA, 1991 and 2011 Realignment, federal grant programs, federal financial participation from Medi-Cal, opioid settlement funds, local funding, and other funding to meet statewide and local outcome measures, reduce disparities, and address the unmet need in their community. In accordance with the BHSA, the IP provides a description of how counties will plan expenditures across a range of behavioral health funding sources and deliver high-quality, culturally responsive, and timely care along the Behavioral Health Care Continuum for the plan period.[2] The Department of Health Care Services (DHCS) is developing an IP Template which will include the required elements for each county to submit in their IPs. A copy of the IP Template will be released in this policy manual to inform county planning. Counties will submit the IP through a DHCS web-based county portal.
IPs require counties to conduct a thorough data-informed local service planning process and provide transparency into county planning for expending BHSA funding and all other behavioral health funding sources overseen by counties. All BHSA services and programming must be planned in accordance with local data. In particular W&I Code section 5963.02, subdivision (b)(2) requires the county to use local substance use disorder (SUD) prevalence data and unmet SUD needs data. IPs will also facilitate local and statewide data collection by providing baseline data on services and planned expenditures and supporting analysis of county goals and outcomes.
A.1 Reporting Period
A draft IP will be due on March 31 for each three-year IP submission. The draft must have a letter from the County Administrative Officer (CAO) approving the draft IP, including the exemption and transfer requests. A final IP is due no later than June 30. County board of supervisor approval is required for submission by June 30.[3] The board of supervisors is also required to confirm in each IP that the county will meet their realignment obligations.[4] The board of supervisors will attest that the county is meeting their realignment obligations, including but not limited to time and distance standards and appointment time standards as set forth W&I Code section 14197.7 without utilizing waitlists, through the Behavioral Health Outcomes, Accountability, and Transparency Report (BHOATR) (see Chapter 4 of this policy manual for BHOATR requirements). The DHCS will post each county’s IP on the DHCS website.
A.2 Contents of Integrated Plan
The IP Template requires counties to report planned activities and projected expenditures for all county behavioral health department services provided under the following funding sources, services, and programs[5]:
Bronzan-McCorquodale Act (1991 Realignment)
2011 Realignment
Medi-Cal behavioral health programs, including:
Specialty Mental Health Services (SMHS)
Drug Medi-Cal (DMC)
Drug Medi-Cal Organized Delivery System (DMC-ODS)
Federal block grants, including:
Community Mental Health Services Block Grant (MHBG)
Substance Use Prevention, Treatment, and Recovery Services Block Grant (SUBG)
Projects for Assistance in Transition from Homelessness (PATH) grant
BHSA funds
Any other federal, state, or local funding directed towards county behavioral health department services, including:
Commercial/private insurance
Opioid settlement funding (only funds received by the County Behavioral Health Department)
County general fund
Grant revenue
Other
The IP Template will include required sections on the following topics:
County Demographics and Behavioral Health Needs
Plan Goals and Objectives
Community Planning Process
Comment Period and Public Hearing
County Behavioral Health Care Continuum Capacity
Services by Total Funding Source
Behavioral Health Services Fund Programs
Workforce Strategy
Budget and Prudent Reserve
A.3 Function of Annual Updates and Intermittent Updates
Counties will be required to update their IP through annual updates in the second and third years of the IP cycle. Annual updates will require the county to complete and submit all sections of the IP. Counties may prepare intermittent updates to their IP at any time during the IP cycle. For intermittent updates, counties must notify DHCS in advance of submission. Annual and intermittent updates will allow counties to be responsive to changes at the local level during the plan period.
Annual and intermittent updates are not subject to the stakeholder engagement requirements for the IP that are outlined in Chapter 3, Section B.1 of this policy manual. However, DHCS encourages stakeholder engagement on the annual and intermittent updates. Counties are required to post the annual updates and intermittent updates to their IP with a summary and justification of the changes made by the updates for a 30-day comment period prior to the effective date of the updates. Counties maintaining their local stakeholder engagement in developing the annual or intermittent updates must continue to comply with the local behavioral health board public hearing requirements outlined in Chapter 3, Section B.3 of this policy manual.
A.3.1 Reporting Period
Counties are required to submit annual updates for the second and third year of the IP period. Draft annual updates will be submitted by March 31 prior to the fiscal year the update will cover. The draft must have a letter from the CAO approving the annual update, including the exemption and transfer requests. A final annual update is due no later than June 30. County board of supervisor approval is required for submission by June 30 prior to the fiscal year the update will cover. Counties may submit intermittent updates to their IP as needed.
Table A.3.1 Reporting Periods for Integrated Plans, Annual Updates, and Intermittent Updates
| Integrated Plan | Annual Updates | Intermittent Updates |
Counties are Required to Complete and Submit [6] | Yes | Yes | If changes are requested |
Submission Timeframe | Every 3 years | Second and third years of IP cycle | Counties may submit at any time |
Submission Deadline for Draft[7] | Draft due March 31 of year prior to fiscal years IP covers | Draft due March 31 of year prior to fiscal year annual update covers | Counties may submit at any time during the 3-year IP cycle |
County Administrative Officer Letter Required | Yes, for draft IP submissions | Yes, for draft annual update submissions | No |
Community Planning Process Required[8] | Yes | No, but encouraged | No, but encouraged |
30-day Public Comment Period Required[9] | Yes | Yes | Yes |
Behavioral Health Board Hearing Required[10] | Yes | If county engages stakeholders | If county engages stakeholders |
Board of Supervisors Approval and Submission[11] | Yes, for final IP, by June 30 | Yes, for final AU, by June 30 | Yes, submitted at any time in FY |
A.3.2 Required Contents
Annual updates will include all sections required in the IP template. If there are no changes to a given section of the county’s IP at the time of the annual update, the county may resubmit the information provided in the original IP as part of the update. Counties may update information in any section of the IP as needed through an intermittent update.
B. Community Planning Process
B.1 Stakeholder Involvement
Stakeholder engagement requirements for the Integrated Plan (IP) are effective January 1, 2025.[12] Counties must engage with local stakeholders to develop each element of their IP.[13] The stakeholders that must be engaged include, but are not limited to[14]:
Eligible adults and older adults[15] (individuals with lived experience)
Families of eligible children and youth, eligible adults, and eligible older adults[16] (families with lived experience)
Youths (individuals with lived experience) or youth mental health or substance use disorder organizations
Providers of mental health services and substance use disorder treatment services
Public safety partners, including county juvenile justice agencies
Local education agencies
Higher education partners
Early childhood organizations
Local public health jurisdictions
County social services and child welfare agencies
Labor representative organizations
Veterans
Representatives from veterans’ organizations
Health care organizations, including hospitals
Health care service plans, including Medi-Cal Managed Care Plans (MCPs)[17]
Disability insurers (a commercial disability insurer that covers hospital, medical or surgical benefits as defined in Insurance Code section 106, subdivision (b))
Tribal and Indian Health Program designees established for Medi-Cal Tribal consultation purposes
The five most populous cities in counties with a population greater than 200,000
Area agencies on aging
Independent living centers
Continuums of care, including representatives from the homeless service provider community
Regional centers
Emergency medical services
Community-based organizations serving culturally and linguistically diverse constituents
In addition to the required stakeholders listed above, stakeholders shall include participation of individuals representing diverse viewpoints,[18] including, but not limited to:
Representatives from youth from historically marginalized communities
Representatives from organizations specializing in working with underserved racially and ethnically diverse communities
Representatives from LGBTQ+ communities
Victims of domestic violence and sexual abuse
People with lived experience of homelessness
Counties are required to demonstrate a partnership with constituents and stakeholders throughout the process that includes meaningful stakeholder involvement on mental health and substance use disorder policy, program planning and implementation, monitoring, workforce, quality improvement, evaluation, health equity, evaluation, and budget allocations.[19] Meaningful stakeholder engagement requires that counties conduct a community planning process that is open to all interested stakeholders and that stakeholders have opportunities to provide feedback on key planning decisions. Stakeholder engagement should not be limited to individuals who belong to organizations or advocacy groups.
Counties must demonstrate a partnership with constituents and stakeholders[20] as part of their community planning processes. Examples of meaningful partnership with stakeholders may include, but are not limited to, the following types of stakeholder engagement:
Education and engagement to support meaningful involvement, including on policies that govern the behavioral health delivery system
Listening sessions
Conference calls
Client advisory meetings
Consumer and family group meetings
Town hall meetings
Video conferences
Media announcements
Targeted Outreach
Public comment
Public hearings
Stakeholder workgroups and committees
Focus groups
Surveys
Key informant interviews or engaging with subject matter experts
Training, education, and outreach related to community planning
Other strategies that demonstrate meaningful partnerships with stakeholders
To ensure that the community planning process is adequately staffed, the county may designate positions and/or units responsible for:
The overall community planning process.
Coordination and management of the community planning process.
Ensuring that stakeholders have the opportunity to meaningfully and sufficiently participate in the community planning process.[21]
Training should be provided by the county as needed to their staff designated responsible for any of the functions that will enable staff to establish and sustain a community planning process.
A county may also provide supports, including, but not limited to, training and technical assistance, to ensure stakeholders, including peers and families, receive sufficient information and data to meaningfully participate in the development of Integrated Plans and annual updates.
Counties may allocate up to 5 percent of the total annual revenue received from the local Behavioral Health Services Fund (BHSF) to fund planning costs.[22] For additional information on how counties can fund the community planning process, please refer to the County Planning Funds Chapter B.4.
B.2 Considerations of Other Local Program Planning Processes
This section focuses on the requirements for Integrated Plan (IP) development related to collaboration with Medi-Cal Managed Care Plans (MCPs) and local health jurisdictions (LHJs).[23] Specifically, the Behavioral Health Services Act (BHSA) requires that each county must:
Work with its LHJ on the development of its Community Health Improvement Plan (CHIP) (W&I Code section 5963.01, subdivision (b)).
Consider the CHIP of each LHJ that covers residents of the county in preparing their IP and annual update (W&I Code section 5963.02, subdivision (b)(4)).
Work with each MCP that covers residents of the county on the development of the MCP’s Population Needs Assessment (PNA) (W&I Code section 5963.01, subdivision (a)).
The BHSA was written prior to the 2024 DHCS redesign of PNA requirements. MCPs no longer develop and submit a PNA to the Department of Health Care Services (DHCS). MCPs now fulfill their PNA requirement by meaningfully participating in the Community Health Assessments (CHA) and CHIPs conducted by LHJs.[24]
Consider the PNA of each MCP that covers residents of the county in preparing their IP and annual update (W&I Code section 5963.02, subdivision (b)(3)).
DHCS is focused on building bridges across public health, MCPs, and behavioral health delivery systems. The BHSA transforms the Mental Health Services Act (MHSA) planning process into a broader county and regional planning process. The targeted points of integrations of BHSA community planning processes with the community- and population-level assessment and planning efforts led by public health with MCPs and other stakeholders will reduce siloes and increase cross-system collaboration to enable strategic alignment of funding for coordinated and complementary approaches. DHCS’ goal is to improve upstream interventions[25] and health outcomes for, and thus more effectively improve the lives of, community members. While perspectives and focus areas may vary, local public health, MCPs, and counties serve common communities, and local integration and partnerships are essential to paving a path toward better understanding the needs of local communities, strategizing appropriate interventions, addressing social determinants of health, and advancing health equity. With this goal in mind, in January 2024, DHCS coordinated with the California Department of Public Health (CDPH) and issued a new policy requiring the MCP PNA to be more closely aligned with LHJ local planning processes, as detailed further below. As the BHSA was written prior to the 2024 DHCS PNA policy change, this guidance explains the BHSA IP requirements in the context of these other recent policy developments.
This guidance addresses requirements for counties’ IP submissions, specific to collaboration with MCPs and LHJs on Community Health Assessments (CHAs) and CHIPs, to promote greater alignment among public health, managed care, and behavioral health.
B.2.1. Local Planning Overview
This section provides background on MCP and LHJ local planning processes.
B.2.1.1 Background: LHJ, CHA, and CHIP
As part of its local planning processes, most LHJs develop both a CHA and a CHIP, which emphasize participatory and collaborative practices centered on the community.[26]
The CHA describes the status of population health within a jurisdiction.[27]
Informed by the CHA, the CHIP identifies how the public health entity will work with community partners to address key issues elevated in the CHA.
An array of tools and processes may be used to conduct a CHA and develop a CHIP; the essential feature is that these processes are informed by community collaboration and participation. Since the CHA and CHIP processes are tailored to address local community needs, there is no requirement to include prescribed topic areas such as specialty or non-specialty mental health, or other content areas.
At present, most LHJs complete or update their CHAs and CHIPs every five years when seeking to obtain and maintain voluntary Public Health Accreditation Board (PHAB) accreditation. Some LHJs are on a three-year submission cycle to align with local processes, such as non-profit hospital community health needs assessments. Currently, non-accredited LHJs can choose not to formally conduct CHAs and CHIPs.
Starting in 2028, as a part of the collaborative state efforts to improve local integration in community planning, the CHA and CHIP will be mandatory for all LHJs, and all LHJs will implement the same three-year submission cycle, as described below in Figure 3.B.2.1. This timeline is intentionally designed to align with and inform BHT IP planning processes as well as simplify the new PNA-CHA policy for MCPs operating in multiple local health jurisdiction areas.
B.2.1.2 Background: MCP PNA
The PNA is the mechanism that MCPs use to identify (1) priority needs of their local communities and members and (2) health disparities. Under the CalAIM Population Health Management (PHM) Program, since January 1, 2024, MCPs have fulfilled their PNA requirement by meaningfully participating in the development of LHJ CHAs and CHIPs in the service areas where MCPs operate.
MCP meaningful participation includes[28]:
Collaboration. MCPs must participate in every LHJ CHA and CHIP in their service area and collaborate with other MCPs within the same service areas to foster a unified planning process.
Data-Sharing. MCPs are expected to share data with LHJs in ways that support the CHA and CHIP process.
Stakeholder Engagement. MCPs must attend key CHA and CHIP meetings and serve on CHA and CHIP governance structures, as requested by LHJs.
Funding and/or In-Kind Staffing. Starting on January 1, 2025, MCPs are required to contribute funding and/or in-kind staffing to support LHJ CHA and CHIP processes.
MCPs are required to complete an “MCP-LHJ Collaboration Worksheet” to demonstrate that they are meeting their PNA requirement.[29]
DHCS and CDPH collaborated to create a regulatory environment that supports effective and efficient joint work on CHAs and CHIPs between LHJs and MCPs. Thus, aligned with CDPH guidance, the cycles for LHJs’ CHA and CHIP development will become standardized across California starting in 2028, as previously noted, and as displayed in the timeline below.
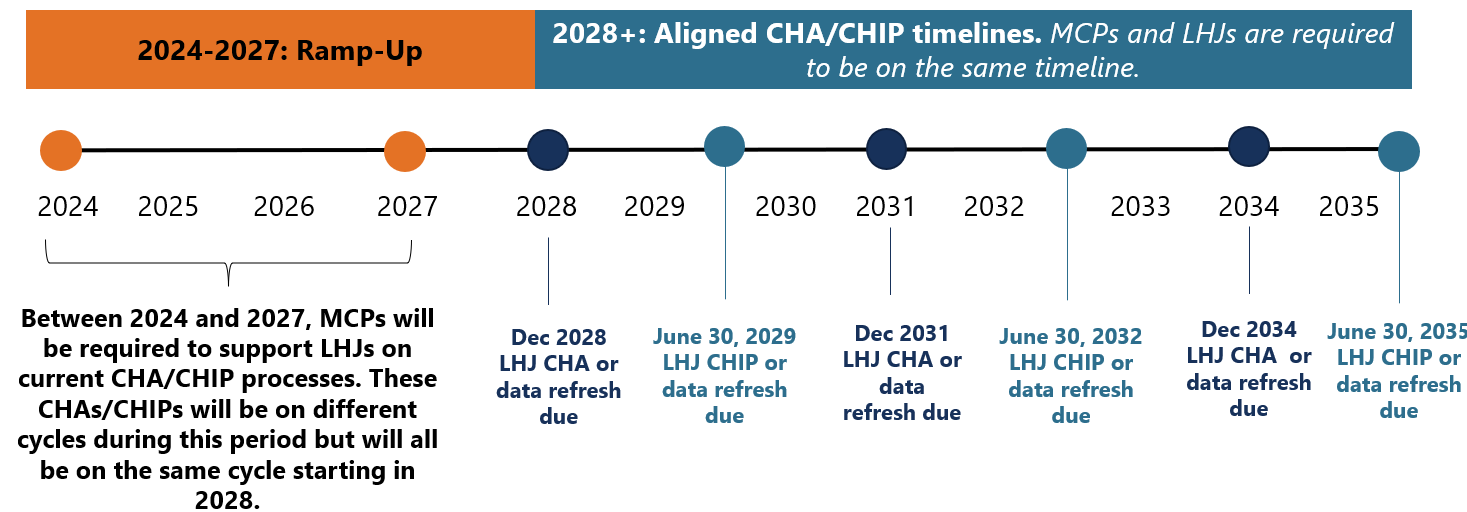
Figure 3.B.2.1. LHJ CHA and CHIP Submission Cycle Alignment Timeline
B.2.2 Overlap and Alignment with Other Local Program Planning Processes
County behavioral health departments (counties), LHJs, and MCPs share a common interest in identifying the needs of the populations and communities they serve. Points of integration existed before SB 326 and its IP mandate, and some counties, LHJs, and MCPs have been collaborating on CHA/CHIP processes for many years.
Specific to BHSA mandates that counties work with and consider LHJ CHAs and CHIPs, and MCP PNAs, DHCS has established the following guiding principles to work toward the achievement of common goals:
Counties, LHJs, and MCPs serve overlapping local communities and should collectively be aware of key, population-level needs and challenges.
There is an opportunity to employ complementary and coordinated strategies and interventions across delivery systems.
As counties begin to engage in the PNA, CHA, and CHIP processes, alignment should lead to more integrated, upstream, and effective community health initiatives and prevention strategies to improve population health.
Given the distinct focus areas and different populations that LHJs, MCPs, and counties serve, DHCS intends for this alignment to supplement the broader county IP requirements.
Figure 3.B.2.2 depicts the initial level of overlap anticipated as counties and LHJs embark on, or in some cases continue, collaborative efforts related to the development and alignment of community needs assessments and planning processes. Additionally, it demonstrates that the IP has numerous requirements unrelated to the LHJ CHA and CHIP. However, over time, as relationships advance, collaboration strengthens, and timelines align, county, MCP, and LHJ overlap on CHAs and CHIPs will likely increase, and the overlap in these circles will expand.
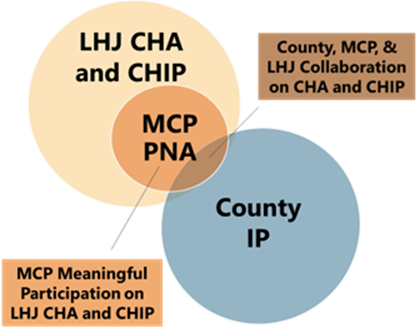
Figure 3.B.2.2 LHJ CHA and CHIP, MCP PNA, and County IP Overlap
B.2.3 County Requirements
This section provides county requirements, effective January 2025, for alignment with LHJs and MCPs in support of the IP submissions due in June 2026.
Engagement with Other Local Program Planning Processes
Counties are required to engage with LHJs and MCPs on CHAs and CHIPs, across the three areas described below. However, given that counties’ IPs and LHJs’ CHAs and CHIPs are driven by unique local needs, DHCS will allow for flexibility in how counties may work with LHJs and MCPs. For example, specific behavioral health topics and focus areas may vary from county to county.
Area 1: Collaboration. Over time, counties, LHJs, and MCPs can partner to focus on coordinated strategies for upstream interventions that can improve population health. To advance meaningful collaboration, counties are required to:
Work with LHJs on the development of the CHA and CHIP in that county (or city, recognizing three city LHJs),[30] along with MCPs, in fulfillment of their meaningful participation requirements. If multiple MCPs are present in the county or city, they will already be aligned in support of the LHJ in accordance with DHCS PHM Policy Guide mandates.
Attend key CHA and CHIP meetings and serve on CHA and CHIP governance structures, including CHA and CHIP subcommittees, at the request of LHJs when discussions are relevant to behavioral health issues.
Area 2: Data-Sharing. Counties, LHJs, and MCPs all have access to their own siloed data. When this data is shared among these partners, it can be used to improve population health by creating a more holistic picture of the multiple factors contributing to a community’s health. Counties are expected to work with LHJs and MCPs to determine the types of relevant data to be shared, taking into consideration the specific nature of CHAs and CHIPs, the needs of the counties, and how data should be de-identified/disaggregated, if needed. Counties are required to begin to identify Statewide Behavioral Health Goals (as described in Chapter 2, Section C.2 Statewide Population Behavioral Health Goals) to:
Share data to support behavioral health-related focus areas of the CHA and CHIP.[31]
Utilize and stratify data from LHJs and MCPs to inform IP development.
Counties are subject to various and specific mandates regarding data sources, uses, and stratification for IP development that exceed the integration of LHJs’ and MCPs’ data. DHCS expects that counties must continue to meet any broader data requirements required by the IP that may not be fulfilled through the LHJ CHA and CHIP processes.
Area 3: Stakeholder Engagement. Given that BHSA identifies more than twenty specific populations and stakeholder groups that counties must engage in the development of the IP, counties should work with LHJs to look for opportunities where IP stakeholder engagement could be combined or integrated with CHA/CHIP processes to reduce duplication and community fatigue. LHJs generally involve a wide array of community stakeholders in the CHA and CHIP development processes. In order to streamline community input and reduce redundancy, counties are required to:
Coordinate stakeholder activities for IP development with LHJ engagement on the CHA and CHIP to the extent possible.
Consider input from diverse populations and a wide range of community stakeholders.
DHCS expects that counties must continue to meet any broader stakeholder engagement requirements that may not be fulfilled through the LHJ CHA and CHIP processes.
Because LHJ stakeholder engagement on CHAs and CHIPs is uniquely focused on the individual needs of each community, there are no prescribed topics or mandated focus areas. However, behavioral health may be a key focus area identified by communities. Counties are expected to participate in the CHA and CHIP as described above, and where behavioral health-specific needs arise through the progress, work with LHJs and MCPs to incorporate addressing such needs in its IP.ar
The county requirements across all three areas noted mirror MCP requirements for meaningful participation on LHJs’ CHAs and CHIPs.[32]
As mentioned previously, due to the current disparate submission cycles for LHJ CHAs and CHIPs, counties should consider the most recent CHA and CHIP on record, which could be up to four years old (depending on the submission cycle) and/or may not be available in all LHJs, when preparing their 2026 IP submissions. For the LHJs without CHAs or CHIPs available, counties should reach out to their respective LHJ to determine if a Strategic Plan is available for their review.
Monitoring and Oversight
In alignment with MCP PNA requirements and to support successful partnerships among counties, LHJs, and MCPs, DHCS has developed, and will require submission of, a “County-LHJ-MCP Collaboration Worksheet” (see Appendix; placeholder- Worksheet to be added when finalized). This Worksheet will require input from all three partners attesting to their efforts across the three areas of collaboration, data sharing, and stakeholder engagement. Completion of the Worksheet will offer insight into these cross-sector partners' experiences as they build relationships and begin working together towards shared goals.
Additionally, LHJs will be separately surveyed to provide their insight on the collaboration with counties.
Iterative Approach for Overlap and Alignment
Figure 3.B.2.3 below details the timeline for implementation of the county, LHJ, and MCP collaboration requirements for the first IP submission in 2026 through the June 2029 IP submission.
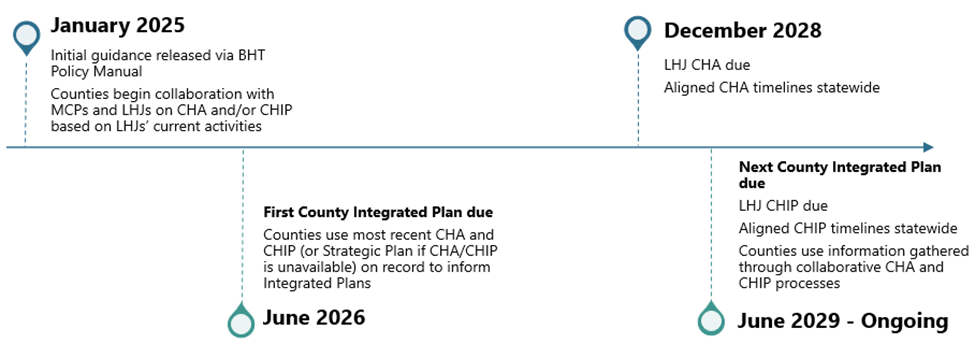
Figure 3.B.2.3 Timeline for Implementation of County, LHJ, and MCP Collaboration
Counties, LHJs, and MCPs should take time in 2025 to come to a common understanding of the respective key facts, goals, and language in each system.
Opportunities should be identified for each entity to share background on their respective requirements and processes (relative to the IP, the PNA, and the CHAs and CHIPs) and how they utilize these tools.
Counties, MCPs, and LHJs should ensure all parties are aligned on one another’s roles and responsibilities, the populations they serve, and the services they are responsible for providing.
B.3 Public Comment and Updates to the Integrated Plan
Comment Period
Counties are required to provide 30 days for stakeholder comment on each draft IP. A draft IP and update shall be prepared and circulated for review and comment for at least 30 days to representatives of stakeholder interests and any interested party who has requested a copy of the draft plans.[33]
Local Behavioral Health Board
The local behavioral health board shall conduct a public hearing on the draft IP at the close of the 30-day comment period.[34]
Once an IP has been drafted and is ready for public comment, the local behavioral health board is required to review the draft plan and make recommendations to the local behavioral health agency for revisions. The local behavioral health board is not required to approve county Integrated Plans.[35]
The local behavioral health agency is also required to provide an annual report to the local governing body, which is the local Board of Supervisors or city council, and DHCS that includes written explanations in response to any substantive recommendations[36] made by the local behavioral health board that are not included in the final IP or update.[37]
Revisions to the Integrated Plan
After the 30-day comment period and public hearing are complete, counties are required to make the following revisions to the IP:
Each draft IP should include a summary of substantive written recommendations.[38]
The draft IP should also include a summary and analysis of the revisions made as a result of stakeholder feedback.[39]
Annual Updates and Intermittent Updates
Counties must prepare annual updates to their IP and may prepare intermittent updates, although intermittent updates are not required. When preparing Annual and Intermittent Updates, counties are not required to comply with the stakeholder process outlined in W&I Code section 5963.03, subdivision (a) and W&I Code section 5963.03, subdivision (b). Counties may choose to elicit participation from stakeholders when preparing annual and intermittent updates. If counties choose to request stakeholder feedback, the county must comply with the local behavioral health board public hearing requirements outlined above.[40]
Counties must post Annual and Intermittent Updates to their IP and a summary and justification of changes to their website for a 30-day comment period prior to the effective date of the updates.[41] Counties will submit annual and intermittent updates to DHCS through the county portal. Counties can download their completed IP from the county portal and submit to the Behavioral Health Services Oversight and Accountability Commission (BHSOAC).
B.4 County Planning Funds
B.4.1 Planning Costs
Counties may allocate up to 5 percent of the total annual revenue received from the local Behavioral Health Services Fund (BHSF) to fund planning costs. All allocations and expenditures for planning costs must be included in the county IP and Behavioral Health Outcomes Accountability and Transparency Report (BHOATR). These planning costs shall include funds for county mental health and substance use disorder programs to pay for the costs of consumers, family members, and other stakeholders to participate in the planning process.[42]
Planning costs may be used to help pay for infrastructure and technologies that will support robust stakeholder engagement. Examples may include but are not limited to:
Laptops and other technologies to help stakeholders participate in the planning process
Web-based meeting platforms
Virtual engagement tools
Accessibility services
Stipends, wages, and contracts to be paid to consumers and family members
Translation/interpretation services
Travel and transportation for stakeholders
Childcare
Eldercare
Training and technical assistance (TTA) for stakeholders to be meaningfully involved including TTA on fiscal policies
Other supports to help with stakeholder engagement
Counties may use planning funds to assess public behavioral health workforce needs required as part of the IP, including the number of providers and vacancies in the county, the county’s ability to develop and maintain a robust workforce that provides adequate access to services and supports, and address statewide behavioral health goals described in Section 2.C of this policy manual. Counties will no longer be required to submit a separate Workforce Needs Assessment beyond what is included in the IP.
Planning costs do not include costs incurred as administrative costs or program expenditures. Additional information on administrative costs, including direct and indirect costs, can be found in Chapter 6.B.
C. Behavioral Health Care Continuum
C.1 Background
Each county’s Integrated Plan (IP) and its associated budget template is required to describe how it will spend behavioral health dollars across a care continuum. Specifically, each county is required to demonstrate, per Welfare and Institutions (W&I) Code section 5963, subdivision (a)(1), how it will:
“utilize various funds for behavioral health services to deliver high quality, culturally responsive, and timely care along the continuum of services in the least restrictive setting from prevention and wellness in schools and other settings to community-based outpatient care, residential care, crisis care, acute care, and housing services and supports.”
To provide counties with more specificity as to what it means to provide care along “the continuum of services,” the California Department of Health Care Services (DHCS) has defined a Behavioral Health Care Continuum. The Behavioral Health Care Continuum is composed of two distinct frameworks for substance use disorder (SUD) and mental health (MH) services. These frameworks will allow counties to describe their expenditures across key service categories, identify gaps in their service continuum, and articulate the investments they will make to expand access, close identified gaps, and improve performance as indicated through statewide behavioral health goals. The use of a standardized Behavioral Health Care Continuum also enables state-level analysis and comparison over time and across counties.[43] The information that counties provide through the Behavioral Health Care Continuum in the IP will not be used to evaluate compliance with expenditure requirements for Behavioral Health Service Act (BHSA) funds.
C.2 Behavioral Health Care Continuum
Counties will report on planned service delivery and expenditures in the IP and budget template, and actual service delivery and expenditures in the Behavioral Health Outcomes, Accountability, and Transparency Report (BHOATR) and expenditure template, disaggregated by child/youth under age 21 and adults aged 21 and older, within the Behavioral Health Care Continuum service categories outlined below. Counties will plan expenditures in the IP by totaling the dollar amount across all behavioral health funding streams for each Behavioral Health Care Continuum service category and will report actual expenditures in the BHOATR by listing the dollar amount from each behavioral health funding stream for each Behavioral Health Care Continuum service category.
The Behavioral Health Care Continuum (shown in Figure 3.C.1) has eight service categories across discrete SUD and MH frameworks, which capture behavioral health programs and services delivered by county behavioral health agencies.[44] One category, Housing Intervention Services, will be reported as a single total across the SUD and MH frameworks within the IP. For the BHOATR, DHCS will ask counties to report actual spending on Housing Intervention Services distinctly in each of the SUD and MH frameworks.

Figure 3.C.1 Behavioral Health Care Continuum
The Behavioral Health Care Continuum does not include county expenditures on: 1) workforce investment activities; 2) capital infrastructure activities; 3) quality and accountability, data analytics, plan management, and administrative activities; and 4) other non-clinical service county behavioral health agency activities (e.g. Public Guardian, forensic activities, Community Assistance, Recovery and Empowerment (CARE) Act). Counties will report these expenditures in the IP and BHOATR distinctly from the Behavioral Health Care Continuum. These non-Continuum expenditure categories will be described in forthcoming guidance on IP and BHOATR reporting.
Tables 3.C.1 and 3.C.2 below describe each of the categories that span the SUD and MH frameworks. The tables below offer descriptions of each service category as well as examples of the specific services that should be reported under the SUD and MH frameworks. A more detailed inventory cataloguing DHCS’s recommended approach to reporting service expenditures across categories in the Behavioral Health Care Continuum will be provided with the release of the IP and BHOATR. Some services, like peer supports, medication services, and case management, may cut across several categories in the Behavioral Health Care Continuum; the funding for these services should be allocated according to the setting in which services are delivered (i.e., peer support services delivered within an outpatient setting should be categorized within “outpatient services”).
SUD and MH frameworks include county reporting on population prevention services. While DHCS recognizes BHSA funds for population prevention are exclusively with the California Department of Public Health (CDPH), counties have other funds that they may use for population prevention (e.g., Substance Abuse and Mental Health Administration (SAMHSA) Substance Use Prevention, Treatment, and Recovery Services Block Grant (SUBG), opioid settlement, Realignment, etc.) which DHCS anticipates this category will capture.
Table 3.C.1 Substance Use Disorder Care Continuum Service Categories, Definitions,[45] and Example Services
Service Categories | Service Category Definition | Example SUD Services[46] |
Population Prevention Services[47] | Includes services and activities that educate and support individuals to prevent substance misuse and substance use disorders from developing. These services/activities offer communities support in identifying and addressing issues, tools for coping with stressors and information on ways to promote resiliency. They may also include services and public health campaigns focused on overdose prevention. |
|
Early Intervention Services[48] | Includes interventions that take a proactive approach to identifying and addressing substance use issues among individuals who are showing early signs, or are at risk, of a substance use disorder. These interventions, such as outreach, access and linkage, and treatment services, help avert the development of a severe and disabling condition, discourage risky behaviors and support individuals in maintaining healthy lifestyles. |
|
Outpatient Services[49] | Includes a variety of therapeutic substance use disorder services that can be provided anywhere an individual is located, such as in school, home, clinic, office, or other outpatient settings. These services may help avert the need for, or be provided after, crisis care, inpatient, or residential treatment. These services are provided, if necessary, as part of stabilization and continued recovery/ongoing evaluation. |
|
Intensive Outpatient Services | Includes services to support individuals living with higher acuity SUD needs who may require assistance at a higher frequency and/or intensity, sometimes via a team-based approach. These services offer structure and monitoring when more support than routine outpatient visits is necessary. |
|
Crisis and Field-Based Services | Includes a range of services that engage, assess, stabilize, treat, and/or coordinate care for individuals in need of substance use disorder services in field settings (e.g., homeless encampments, shelters, or syringe service programs). Services may be delivered in non-traditional settings where individuals work or reside. |
|
Residential Treatment Services | Includes low- to high-intensity clinically managed residential treatment. Services may be delivered in short-term residential settings of any size. |
|
Inpatient Services | Includes 24-hour, intensive treatment services to individuals who require medical management or medical monitoring for substance use disorder needs. |
|
Housing Intervention Services (reporting is aggregated with the mental health framework) | Includes services and supports designed to enable individuals to remain in their homes or obtain housing to support recovery and improved health outcomes. Services help individuals find and retain housing, support recovery and resiliency, and/or maximize the ability to live in the community. |
|
Table 3.C.2 Mental Health Care Continuum Service Categories, Definitions,[51] and Example Services
Service Categories | Service Category Definition | Example MH Services |
Population Prevention Services | Includes services and activities that educate and support individuals to prevent acute or chronic conditions related to mental health from ever developing. These services/activities may offer communities support in identifying and addressing issues before they turn into problems, tools for coping with stressors and information on ways to promote resiliency. |
|
Early Intervention Services[52] | Includes interventions that take a proactive approach to identifying and addressing mental health issues among individuals who are showing early signs, or are at risk, of a mental health disorder. These interventions, such as outreach, access and linkage, and treatment services, help avert the development of a severe and disabling condition, discourage risky behaviors and support individuals in maintaining healthy lifestyles. |
|
Outpatient[53] & Intensive Outpatient Services | Includes a variety of therapeutic mental health services that can be provided anywhere an individual is located, such as in school, home, clinic, office, field settings (e.g. homeless encampments, shelters, etc.) or other outpatient settings. Also includes services to support individuals living with higher acuity mental health needs who may require assistance at a higher frequency and/or intensity, sometimes via a team-based approach. These services may help avert the need for, or be provided after, crisis care, inpatient or residential treatment and are provided, if necessary, as part of stabilization and continued recovery/ongoing evaluation. They may also offer structure and monitoring when more support than routine outpatient visits is necessary. |
|
Crisis Services | Includes a range of services and supports that assess, stabilize, and treat individuals experiencing acute distress. Services are designed to provide relief to individuals experiencing a mental health crisis, including through de-escalation and stabilization techniques, and may be delivered in clinical and non-clinical settings. |
|
Residential Treatment Services | Includes intensive treatment services that are provided in a structured, facility-based setting to individuals who require consistent monitoring for mental health needs on a longer-term basis. Services may be delivered in short-term residential settings to divert individuals from or as a step-down from hospital and acute services. |
|
Hospital and Acute Services | Includes treatment services that are provided in structured, hospital settings to individuals who require consistent monitoring and stabilization. These services may include comprehensive psychiatric treatment, including medication adjustments, and acute withdrawal services. |
|
Subacute and Long-Term Care Services | Includes intensive licensed skilled nursing care provided to patients with mental health needs, most frequently delivered in a skilled nursing facility (SNF) and special treatment programs (STPs). |
|
Housing Intervention Services (reporting is aggregated with the substance use disorder framework) | Includes services and supports designed to enable individuals to remain in their homes or obtain housing to support recovery and improved health outcomes. Services help individuals find and retain housing, support recovery and resiliency, and/or maximize the ability to live in the community. |
|
D. County Integrated Plan Alignment with Statewide Population Behavioral Health Goals
As outlined in W&I Code section 5963.02, subdivision (c)(3)(A), each county shall develop an Integrated Plan (IP) and annual update (AU) aligned with their associated measures. DHCS will identify and provide counties with measures of their performance relative to the statewide behavioral health goals. Counties will use those measures to inform resource planning in their IPs and AUs, as well as their approach to population health management and implementation of targeted interventions to drive progress on statewide behavioral health goals. In forthcoming guidance, DHCS will describe its approach to calculating performance measures and delineate expectations for counties, MCPs, and other stakeholders as part of a monitoring and accountability framework. See Section 2.C for more detailed information.
[1] W&I Code §§ 5963, subdivision (a); 5963.02, subdivision (a)
[2] W&I Code § 5963, subdivision (a)(1)
[3] W&I Code § 5963.02, subdivision (a)(3)
[4] W&I Code § 14197.71, subdivision (c)(2)
[5] W&I Code § 5963.02, subdivision (c)(1-2)
[6] W&I Code § 5963.02, subdivision (a)(1)
[7] W&I Code § 5963.02, subdivision (a)(3)
[8] W&I Code § 5963.03, subdivision (a)
[9] W&I Code § 5963.03, subdivision (c)(B)
[10] W&I Code § 5963.03, subdivision (b)
[11] W&I Code §§ 5963.03, subdivision (c)(10)-(11)
[12] W&I Code §5963.03, subdivision (e)
[13] W&I Code §5963.02, subdivision (c)
[14] W&I Code §5963.03, subdivision (a)(1)
[15] W&I Code § 5892, subdivision (d)(1)
[16] W&I Code § 5892, subdivision (d)
[17] W&I Code § 14184.101, subdivision (j)
[18] W&I Code § 5963.03, subdivision (a)(2)(A)(ii)
[19] W&I Code § 5963.03(a)(2)(A)(i)
[20] W&I Code § 5963.03, subdivision (a)(2)(A)(i)
[21] W&I Code §5963.03, subdivisions (a)(2)(A)(i) and (ii)
[22] W&I Code §5892, subdivision (e)(1)
[23] Per HSC Section 124030, subdivision (f) a “Local health jurisdiction” means county health department or combined health department in the case of counties acting jointly or city health department within the meaning of HSC §101185.
[24] CalAIM: Population Health Management Policy Guide (May 2024)
[25] Upstream interventions include those that link to public health and social services and support members staying healthy through wellness and prevention services. For further details and additional context, see the PHM Policy Guide (p.4) and CalAIM Population Health Management Initiative webpage.
[26] For further details and additional context, see the California Department of Public Health December 26, 2023 Memo to All Local Health Jurisdictions and the CalAIM PHM Policy Guide (p. 8-10)
[27] Although the BHSA does not specifically reference the CHA and only the CHIP, the CHA and CHIP are part of the same local LHJ planning process, and the CHA is the essential precursor step to developing the CHIP.
[28] See the CalAIM PHM Policy Guide for additional details on MCP PNA Requirements (p. 7-10)
[29] MCPs are not required to submit MCP-LHJ Collaboration Worksheet unless requested by DHCS. In addition, all MCPs are required to submit a PHM Strategy which provides details on MCPs’ meaningful participation on LHJs’ CHA and CHIP.
[30] For a complete list of LHJs, see CDPH’s listing of local health services/offices.
[31] Counties will need to adhere to applicable federal and state privacy laws and regulations (e.g., consent requirements) and relevant frameworks (e.g. the California Health and Human Services Agency Data Exchange Framework if county is a signatory) while fulfilling the BHSA requirements to share and utilize data, as will MCPs and LHJs. BHSA includes broader data sharing and utilization requirements that counties must fulfill for their IP submissions.
[32] DHCS does not require or expect counties to provide funding and/or in-kind staffing to support the LHJ CHA and CHIP processes. Per the PHM Policy Guide, however, MCPs are required to work with LHJs to determine what combination of funding and/or in-kind staffing the MCP will contribute to the LHJ CHA/CHIP process.
[33] W&I Code § 5963.03, subdivision (a)(2)(B)
[34] W&I Code § 5963.03, subdivision (b)(1)
[35] W&I Code § 5963.03, subdivision (b)
[36] W&I Code § 5963.03, subdivision (d)
[37] W&I Code §5963.03, subdivision (b)(5)
[38] W&I Code § 5963.04, subdivision (d)
[39] W&I Code § 5963.03, subdivision (b)(3)
[40] W&I Code § 5963.03, subdivision (b)(1)
[41] W&I Code § 5963.03, subdivision (c)(2)(B)
[42] W&I Code § 5892, subdivision (e)(1)(B)-(C)
[43] While informed by national behavioral health frameworks, the Behavioral Health Care Continuum is tailored to California’s specific landscape and adjusted to reflect input from California stakeholders. The Continuum is also informed by DHCS's previous assessment of California's Medi-Cal behavioral health service delivery system.
[44] The Behavioral Health Care Continuum includes services provided in facilities designated as Institutions for Mental Disease (IMD) and services in non-IMD facilities. The IMD exclusion is only applicable to billing for Medi-Cal services.
[45] Definitions are informed by DHCS's previous assessment of California's Medi-Cal behavioral health service delivery system and tailored to the county landscape.
[46] Services referenced reflect the ASAM 3rd edition. Medi-Cal guidance on the ASAM 4th edition is forthcoming. Available here.
[47] While BHSA funds for population prevention are exclusively with the California Department of Public Health (CDPH), counties have other funds that they may use for population prevention (e.g., SAMHSA SUBG block grant, opioid settlement, Realignment, etc.) which this category will capture.
[48] W&I Code § 5840, subdivisions (b)(1)-(3)
[49] W&I Code § 5887, subdivision (a)(4)
[50] W&I Code § 5887, subdivision (a)(3)
[51] Definitions are informed by DHCS's previous assessment of California's Medi-Cal behavioral health service delivery system and tailored to the county landscape.
[52] W&I Code § 5840, subdivisions (b)(1)-(3)
[53] W&I Code § 5887, subdivision (a)(4)
