9. Appendix
A: Select Definitions
1. Experiencing Homelessness
An individual or family who lacks a fixed, regular, and adequate nighttime residence, meaning:
An individual or family with a primary nighttime residence that is a public or private place not designed for or ordinarily used as a regular sleeping accommodation for human beings, including a car, park, abandoned building, bus or train station, airport, or camping ground;
An individual or family living in a supervised publicly or privately operated shelter designated to provide temporary living arrangements (including congregate shelters, transitional housing, and hotels and motels paid for by charitable organizations or by federal, state, or local government programs for low-income individuals); or
An individual who is exiting an institution and was considered homeless immediately prior to entering the institution or becomes homeless during the institutional stay, regardless of the length of stay.
An individual or family who will imminently lose their primary nighttime residence, provided that:
The primary nighttime residence will be lost within 30 days of the date of application for homeless assistance;
No subsequent residence has been identified; and
The individual or family lacks the resources or support networks, e.g., family, friends, faith-based or other social networks, needed to obtain other permanent housing.
Unaccompanied youth under 25 years of age, or families with children and youth, who do not otherwise qualify as homeless under this definition, but who:
Are defined as homeless under section 387 of the Runaway and Homeless Youth Act (42 U.S.C. 5732a), section 637 of the Head Start Act (42 U.S.C. 9832), section 41403 of the Violence Against Women Act of 1994 (42 U.S.C. 14043e-2), section 330(h) of the Public Health Service Act (42 U.S.C. 254b(h)), section 3 of the Food and Nutrition Act of 2008 (7 U.S.C. 2012), section 17(b) of the Child Nutrition Act of 1966 (42 U.S.C. 1786(b)), or section 725 of the McKinney-Vento Homeless Assistance Act (42 U.S.C. 11434a);
Have not had a lease, ownership interest, or occupancy agreement in permanent housing at any time during the 60 days immediately preceding the date of application for homeless assistance;
Have experienced persistent instability as measured by two moves or more during the 60-day period immediately preceding the date of applying for homeless assistance; and
Can be expected to continue in such status for an extended period of time because of chronic disabilities, chronic physical health or mental health conditions, substance addiction, histories of domestic violence or childhood abuse (including neglect), the presence of a child or youth with a disability, or two or more barriers to employment, which include the lack of a high school degree or General Education Development (GED), illiteracy, low English proficiency, a history of incarceration or detention for criminal activity, and a history of unstable employment.
Any individual or family who:
Is fleeing, or is attempting to flee, domestic violence, dating violence, sexual assault, stalking, or other dangerous or life-threatening conditions that relate to violence against the individual or a family member, including a child, that has either taken place within the individual's or family's primary nighttime residence or has made the individual or family afraid to return to their primary nighttime residence;
Has no other residence; and
Lacks the resources or support networks, e.g., family, friends, faith-based or other social networks, to obtain other permanent housing.
2. At-Risk of Homelessness
An individual or family who:
Does not have sufficient resources or support networks, e.g., family, friends, faith-based or other social networks, immediately available to prevent them from moving to an emergency shelter or another place described in paragraph (1) of the “Homeless” definition in this section; and
Meets one of the following conditions:
Has moved because of economic reasons two or more times during the 60 days immediately preceding the application for homelessness prevention assistance;
Is living in the home of another because of economic hardship;
Has been notified in writing that their right to occupy their current housing or living situation will be terminated within 30 days after the date of application for assistance;
Lives in a hotel or motel and the cost of the hotel or motel stay is not paid by charitable organizations or by federal, state, or local government programs for low-income individuals;
Lives in a single-room occupancy or efficiency apartment unit in which there reside more than two persons or lives in a larger housing unit in which there reside more than 1.5 people per room, as defined by the U.S. Census Bureau;
Is exiting a publicly funded institution, or system of care (such as a health-care facility, a mental health facility, foster care or other youth facility, or correction program or institution); or
Otherwise lives in housing that has characteristics associated with instability and an increased risk of homelessness, as identified in the recipient's approved consolidated plan.
A child or youth who does not qualify as “homeless” under this section, but qualifies as “homeless” under section 387(3) of the Runaway and Homeless Youth Act (42 U.S.C. 5732a(3)), section 637(11) of the Head Start Act (42 U.S.C. 9832(11)), section 41403(6) of the Violence Against Women Act of 1994 (42 U.S.C. 14043e-2(6)), section 330(h)(5)(A) of the Public Health Service Act (42 U.S.C. 254b(h)(5)(A)), section 3(m) of the Food and Nutrition Act of 2008 (7 U.S.C. 2012(m)), or section 17(b)(15) of the Child Nutrition Act of 1966 (42 U.S.C. 1786(b)(15)); or
A child or youth who does not qualify as “homeless” under this section, but qualifies as “homeless” under section 725(2) of the McKinney-Vento Homeless Assistance Act (42 U.S.C. 11434a(2)), and the parent(s) or guardian(s) of that child or youth if living with her or him.
3. Chronically Homeless
A homeless individual with a disability as defined in section 401, subdivision (9) of the McKinney-Vento Assistance Act (42 U.S.C. section 11360, subdivision (9)), who:
Lives in a place not meant for human habitation, a safe haven, or in an emergency shelter, and
Has been homeless as defined in 7.C.4.1.1 Experiencing Homelessness and At Risk of Homelessness on any number of occasions in the last 3 years, as long as the combined occasions equal at least 12 months; or
An individual who is exiting an institution and met all of the criteria in paragraph (1) immediately prior to entering the institution regardless of the length of stay; or
A family with an adult head of household (or, if there is no adult in the family, a minor head of household) who meets all of the criteria in paragraph (1) or (2), including a family whose composition has fluctuated while the head of household has been homeless.
B: Coverage of Settings
Assisted Living | Community Residential Treatment (Settings eligible under BHCIP) | Interim Housing | Housing | |
Settings |
|
| ||
BHT Housing Interventions | Yes | Peer respite only | Yes, can be used for an additional 6 months if member is receiving Transitional Rent under managed care or up to 12 months if member is not eligible for Transitional Rent. The aim is to transition individuals to permanent housing as quickly as possible. | Yes[7] |
Transitional Rent | No | Peer respite, when provided as transitional or recovery housing including bridge, site-based, population-specific, and community living programs that may or may not offer supportive services and programming | Yes (see note) ~Note: Transitional rent is not available for Recuperative Care and Short-Term Post-Hospitalization. | Yes |
Appendix C: Promoting Access to Care through Efficient use of State and County Resources Appendices
1. Process Flow for Behavioral Health Services Act-Funded Providers: Checking for and Billing Medi-Cal or Other Health Coverage
Appendix Figures C.1.1 and C.1.2 below bring together the requirements in overarching process flows for providers when seeking to bill Medi-Cal or Other Health Coverage. Appendix Figure C.1.1 displays the process for a Behavioral Health Services Act (BHSA)-funded provider to determine whether or not to check an individual’s insurance coverage (public or commercial) in accordance with the policy described in this manual.
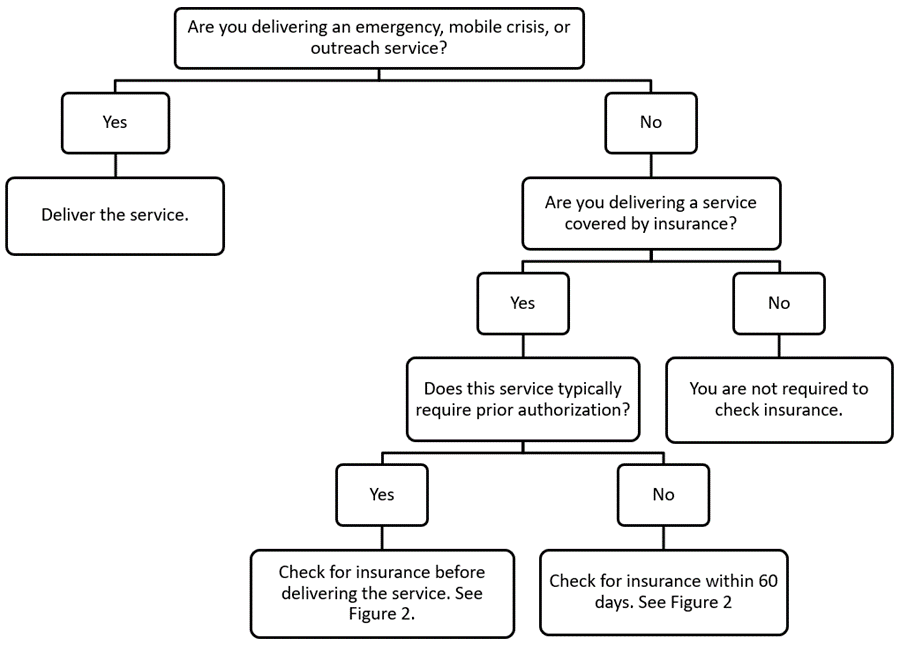
Appendix Figure C.1.1. Process flow to determine if BHSA-funded provider must check for an individual‘s insurance coverage.
For BHSA-funded providers who must check for public or commercial insurance as determined by Appendix Figure C.1.1 above, Appendix Figure C.1.2 is a process flow for individual BHSA-funded providers to check for and bill for public or commercial insurance.
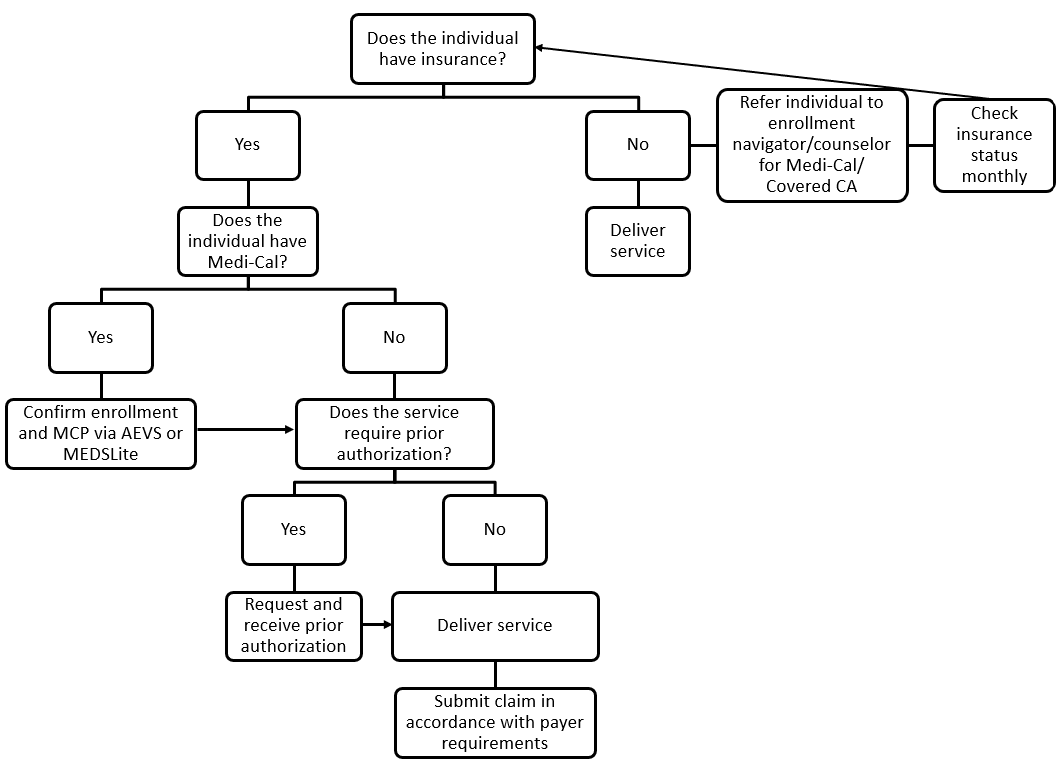
Appendix Figure C.1.2. Process flow for BHSA-funded provider to check for and bill Medi-Cal or commercial insurance.
Commercial insurers require prior authorization for most services. In the event a provider obtains an individual’s insurance information after the service, the provider may still pursue payment by seeking authorization and submitting a claim.
2. Medi-Cal Billing and Documentation Resources
The Department of Health Care Services (DHCS) acknowledges that standard Medi-Cal billing procedures outlined in Policy C.2.3 (Consistently Bill Medi-Cal) may be new for some providers. To support these providers, DHCS is providing a table summarizing current billing and documentation resources for Medi-Cal enrolled providers. DHCS also reminds counties that the fiscal policies outlined in this chapter do not supersede baseline licensing, certification, and credentialing requirements before a provider may deliver and/or bill Medi-Cal for behavioral health services.[8] All providers—Behavioral Health Services Act (BHSA)-funded or otherwise—must continue to meet applicable requirements
Appendix Table C.2.1: Resources for Medi-Cal Billing and Documentation Requirements
Type of Resource | Description |
DHCS |
|
Authorization Resources |
|
Documentation Resources |
|
California Mental Health Services Administration (CalMHSA) Resources |
|
Managed Care Plan (MCP) Resources |
|
For specific Medi-Cal billing questions, providers may contact the Telephone Service Center, (800) 541-5555 (outside of California, 916-636-1980) or online at Contact Medi-Cal. | |
3. Commercial Health Insurance Billing Guidance and Resources
When a commercially insured individual receives a BHSA-funded service that is covered or can be paid by the individual’s commercial plan, counties must require that providers make a good faith effort to seek payment from the commercial plan.[9] This section provides additional detail for counties to support providers in consistently billing commercial health insurance (Policy C.3.2).
Contact the individual’s commercial health plan for non-emergency services to confirm the following by calling the commercial health plan’s provider services number listed on the member’s identification (ID) card or the plans’ webpage for providers. Have the member’s name, date of birth, and ID number(s) available when you ask about:
Whether the plan covers this service provided by an out-of-network provider when prior authorization is obtained. If not, skip remaining steps and use BHSA funds.
Whether prior authorization is required. If so, submit a prior authorization request. (See below for additional discussion of prior authorization.)
What other billing and coding requirements apply for this service, including:
Billing procedures
Which billing codes to use
Documentation requirements
Special requirements for out-of-network billing, such as a specific billing form.
For higher-cost or longer-term services (such as inpatient detoxification or a residential program), what coverage limits the plan imposes (e.g., max covered days, or a requirement to request continuing authorization after a certain number of days), and whether the plan will pay the provider’s standard rate.
If the plan does not provide a clear answer or has a default rate significantly below the provider’s standard rate, make a good faith effort to execute a single case agreement (as described below).
For an out-of-network provider to implement this policy after providing a service:
Submit a complete claim in accordance with Health and Safety Code section 1371.35 and the commercial plan’s requirements (e.g., using the plan’s form for out-of-network billing, using the plan’s required billing codes, or attaching any required documentation such as a prior authorization or single case agreement).
Bill at the provider’s standard rate. The commercial plan may or may not agree to pay this rate,[10] unless the provider and plan previously executed a single case or letter of agreement.
If the plan denies the claim, pays less than the agreed-upon amount, or delays payment past the legal deadline, pursue the plan’s dispute resolution process[11] and file a complaint with the state (as described below).
Prior Authorization. As under Medi-Cal, each health plan sets requirements for which services and prescription drugs require prior authorization, what information must be included in a request for prior authorization, and how prior authorization requests must be submitted.
As the name suggests, prior authorization must be requested before the service is provided. If a provider furnishes services without seeking prior authorization, the plan will typically deny the claim, even if the provider otherwise complied with all applicable requirements. Additional notes on prior authorization:
Prior authorization requirements are more common for higher-cost services than for lower-cost services and are more often required for out-of-network providers than for in-network providers.
California requires health insurance plans to use prior authorization processes that assure the provision of covered services in a timely manner.[12]
Depending on the plan, providers may be required or permitted to submit prior authorization requirements by mail, fax, and/or electronically. Providers may also need to check the status of the prior authorization request through plan-specific online portals.[13]
Single Case Agreements, Letters of Agreement, and Network Contracts. Under certain circumstances, it may be most effective or efficient for an out-of-network provider to establish a more formal agreement with a commercial plan rather than simply submitting claims for out-of-network payment. These circumstances may include a treatment plan involving longer-term services (e.g., weekly services for several months) or higher-cost services (e.g., crisis, residential, or inpatient services). In addition, an agreement or contract with the health plan may be helpful to ensure claims are paid timely and at the agreed upon rate(s).
In these scenarios, the Department of Health Care Services (DHCS) encourages counties and providers to consider the following potential approaches:
Single Case Agreement:[14] This type of agreement describes the terms of coverage and payment for an out-of-network provider delivering a single course of treatment to a single patient. These agreements are typically negotiated after the provider receives prior authorization for a service and/or before the provider begins furnishing services. However, each plan has its own policies and procedures for negotiating single case agreements.
Letter of Agreement:[15] This type of agreement between a plan and out-of- network provider aims to avoid the need for multiple single case agreements. It may be used where a provider expects to treat multiple patients from the same plan, or where a single patient may need ongoing treatment over a longer time horizon, making it inefficient to continually amend the single case agreement to accommodate the evolving treatment plan. Like a single case agreement, letters of agreement define the terms of coverage and payment.
Network Participation Request from the Provider: If a BHSA-funded provider has seen, or expects to see, multiple patients served by the same plan, it may be prudent for the provider to request to join the plan’s provider network. DHCS expects this strategy may be more appropriate for larger providers offering clinical services covered under California’s parity law and/or mobile crisis services as required by Senate Bill (SB) 855 and Assembly Bill (AB) 988.[16] By participating in the plan’s network, the provider would bypass many coverage restrictions and procedural requirements applicable to out-of-network providers. In addition, after being added to the plan’s provider directory, the provider may gain additional individuals covered by the plan. Most plans’ provider websites include information about requesting to join the plan’s network.
County-Facilitated Network Participation: Counties could explore the possibility of contracting with a commercial health plan on behalf of a group of BHSA-funded providers offering clinical or mobile crisis services (potentially including both county-operated and county-contracted providers). To pursue this option, counties may need to secure authorization from contracted providers to negotiate with plans on their behalf.
4. Other Non-Behavioral Health Services Act Funds Guidance and Resources
The fiscal policy outlined in Chapter 6, Section C.4 applies to the additional sources of funding that county behavioral health agencies utilize to deliver behavioral health services and supports other than Medi-Cal federal financial participation (FFP) and commercial insurance. The sources of funding are listed in Chapter 6, Section C.4 and described further below.
State funds, including:
Opioid settlement funds, as described in the California Opioid Settlements Allowable Expenditures resource.[19]
Federal grants, including:
Block grants issued by the Substance Abuse and Mental Health Services Administration (SAMHSA), such as:
The Community Mental Health Services Block Grant (MHBG), which supports efforts to establish or expand an organized community-based system of care for providing mental health services to children living with serious emotional disturbances and adults living with serious mental illness.[20]
The Substance Use Prevention, Treatment and Recovery Services Block Grant (SUBG, and referred to under federal law as SUPTBG), which funds authorized SUD prevention, treatment, and recovery support services.[21]
Projects for Assistance in Transition from Homelessness (SAMHSA PATH), a federal matching grant that funds community based-outreach, mental health and substance abuse referral/treatment, case management, and other support services, as well as a limited set of housing services for adults who are homeless or at imminent risk of homelessness and have a serious mental illness.[22]
Other sources of funding, not otherwise mentioned, that county behavioral health agencies use to deliver services, such as non-federal grants and county general funds, and revenues collected from any fines or fees levied (such as those deposited in county Maddy and Statham funds, respectively), private grants, and community benefit funding from health systems.
Appendix D: Policy Manual Definitions
Behavioral Health Bridge Housing (BHBH): BHBH provides over a billion dollars in funding to county behavioral health agencies and tribal entities to operate bridge housing settings to address the immediate housing needs of people experiencing homelessness who have serious behavioral health conditions. The BHBH program was signed into law in September 2022 under Assembly Bill 179 and provides funding through June 30, 2027. Reference: Assembly Bill 179, 2022; Senate Bill 107, 2024; BHBH
Behavioral health services: “Behavioral health services” means mental health services and substance use disorder treatment services, as defined in Section 5891.5. Reference: W&I Code section 5892, subdivision (k)(1).
California Environmental Quality Act (CEQA): The California Environmental Quality Act generally requires state and local government agencies to inform decision makers and the public about the potential environmental impacts of proposed projects, and to reduce those environmental impacts to the extent feasible. The laws and rules governing the CEQA process are contained in the CEQA statute (Public Resources Code Section 21000 and following), the CEQA Guidelines (California Code of Regulations, Title 14, Section 15000 and following), published court decisions interpreting CEQA, and locally adopted CEQA procedures. References: Public Resources Code Section 21000 and following; California Code of Regulations, Title 14, Section 15000 and following; California Environmental Quality Act
Commercial health plan: “Commercial health plan” means an individual health plan purchased on Covered California, or a group health plan sponsored by an employer, including both state-regulated group health plans and self-insured group health plans governed by the Employee Retirement and Income Security Act (ERISA). This term includes commercial plans regulated by both Department of Managed Health Care and California Department of Insurance. Reference: DMHC; Covered California; California Department of Insurance
Community Health Assessment (CHA): CHA is an assessment conducted by local health jurisdictions to systematically examine the health status indicators for a given population that is used to identify key problems and assets in a community. Reference: DHCS PHM Policy Guide; Alignment of Medi-Cal Managed Care Population Needs Assessment and Local Health Jurisdiction Community Health Assessments and Community Health Improvement Plans; Public Health Accreditation Board Standards and Measures
Community Health Improvement Plan (CHIP): CHIP is the output of the Community Health Assessment. The Community Health Improvement Plan is the action plan developed by Local Health Jurisdictions for how a community will use the data identified in the Community Health Assessment to improve health outcomes. Reference: DHCS PHM Policy Guide; Alignment of Medi-Cal Managed Care Population Needs Assessment and Local Health Jurisdiction Community Health Assessments and Community Health Improvement Plans; Public Health Accreditation Board Standards and Measures; W&I Section 5963.02, subdivision (b)(4)
Community-defined evidence-based practice (CDEP): CDEPs are an alternative or complement to evidence-based practices, that offers culturally anchored interventions that reflect the values histories and life experiences of the communities that the provider is providing services to. These practices come from the community and the organizations that serve them and are found to yield positive results as determined by community consensus over time. Reference: W&I Code 5892, subdivision (k)(6)
Continuums of Care (CoCs): A regional or local planning body that coordinates housing and services funding for families and individuals experiencing homelessness. It is responsible for carrying out the responsibilities required under the CoC Program Interim Rule, including selecting a Homeless Management Information software solution and a Homeless Management Information System Lead. Reference: HUD Continuum of Care Program
County: “County” means the County Behavioral Health Department, two or more County Behavioral Health Departments acting jointly, and/or city-operated programs receiving funds pursuant to W&I Code 5701.5 References: W&I Code 5849.2, subdivision (f); W&I Code 5701.5
Culturally responsive and linguistically appropriate: Culturally responsive and linguistically appropriate refers to the ability to reach underserved cultural populations and address specific barriers related to racial, ethnic, cultural, language, gender, gender identity, sexual orientation, age, economic, or other disparities in mental health and substance use disorder treatment services access, quality, and outcomes. Reference: W&I Code 5840.6, subdivision (f)(1)
Department: “Department” means the State Department of Health Care Services. Reference: W&I Code 5963 subdivision (b)(2)
Evidence-based practice (EBP): EBPs are those with documented, empirical evidence (e.g., randomly controlled trials, peer-reviewed studies, and publications) of effectiveness in improving behavioral health. These programs and practices have been clinically reviewed and codified, meaning the practices have been manualized to ensure the fidelity of implementation in a variety of settings. At both the federal and state level, there are existing databases of EBP resources through the Substance Abuse and Mental Health Services Administration (SAMHSA) and the California Evidence-Based Clearinghouse for Child Welfare (CEBC), respectively. Reference: DHCS CYBHI Grant Strategy, 2022
Homeless Management Information System (HMIS): HMIS is a local information technology system used to collect individual-, program-, and organization-level data on the provision of housing and services to individuals and families at risk of and experiencing homelessness. Continuums of Care are responsible for selecting an HMIS software solution that complies with HUD standards. Reference: W&I Code Section 8256; HMIS Requirements
HMIS Common Data Elements: Also referred to as Common Program Specific Data Elements, the common data elements have been cooperatively developed by HMIS Federal Partners and have multiple response categories for each element. Reference: HMIS Data Standards Manual
HMIS Universal Data Elements: HMIS Universal Data Elements are elements required to be collected by all projects participating in HMIS, regardless of funding source. Reference: HMIS Data Standards Manual
Local Health Jurisdiction (LHJ): “LHJ” means county health department or combined health department in the case of counties acting jointly or city health department within the meaning of Section 101185. Reference: (CA Health & Safety Code Section 124030(f)) & DHCSDOC-2067478743-514 (http://ca.gov ); W&I Section 5963.01 subdivision (b)
Medi-Cal Behavioral Health Delivery System: An entity or local agency that contracts with the department to provide covered behavioral health Medi-Cal benefits, including Medi-Cal Specialty Mental Health Services (SMHS), Drug Medi-Cal (DMC), and/or Drug Medi-Cal Organized Delivery System (DMC-ODS). Reference: W&I Code section 14184.101 subdivision (i)
Medi-Cal Managed Care Plan (MCP): “Medi-Cal Managed Care Plan” means any individual, organization, or entity that enters into a comprehensive risk contract with the department to provide covered full-scope health care services to enrolled Medi-Cal beneficiaries pursuant to any provision of this chapter or Chapter 8 (commencing with Section 14200). Reference: W&I Code section 14184.101 subdivision (j)
Out-of-Network Provider: “Out-of-network provider” means a provider or group of providers who does not have a network provider agreement with the relevant public health insurance agency (e.g., DHCS or a County Behavioral Health Agency) or commercial health plan. A provider may be “out of network” for one insurance network but in the network with another one.
Population Needs Assessment (PNA): PNA is the mechanism that Medi-Cal Managed Care Plans use to identify the priority needs of their local communities and members and to identify health disparities. Reference: DHCS PHM Policy Guide; W&I Section 5963.02 subdivision (b)(3)
Prudent Reserve: The prudent reserve is an account that counties may transfer a portion of their Behavioral Health Services fund monies into to ensure that the county can continue to provide services at the same level if their future funding decreases. References: W&I Code sections 5892(b)(1); 5892(b)(3); 5892(b)(4); and 5892(b)(5)(A)
Reversion: Reversion refers to the process in which, other than Prudent Reserve dollars, Behavioral Health Services Act (BHSA) funds that are allocated to a county by the State Controller must be spent within a certain time period or the funds will revert back to DHCS for reallocation to other counties for future use. References: W&I Code 5892(b)(1); 5892(b)(3); 5892(b)(4); and 5892(b)(5)(A)
Single Case Agreement: “Single case agreement”, sometimes referred to as a letter of agreement, means an agreement for reimbursement reflecting the terms and conditions of payment, including the payment amount, between a plan and provider for one episode of care for one patient, when the provider is out-of-network or the treatment is not covered under the patient’s plan. Agreements may be developed with Medi-Cal Managed Care Plans (MCPs), commercial health plans, and/or other health plans that differentiate in-network and out-of-network service providers.
Substance Use Disorder: Substance use disorder means an adult, child, or youth who has at least one diagnosis of a moderate or severe substance use disorder from the most current version of the Diagnostic and Statistical Manual of Mental Disorders for Substance-Related and Addictive Disorders, with the exception of tobacco-related disorders and non-substance-related disorders. For purposes of this manual, substance use disorder treatment services include harm reduction, treatment, and recovery services, including all federal Food and Drug Administration approved medications. Reference: W&I Code 5892(k)(1), 5891.5(b)(2).
Subcontractor: “Subcontractor” means an individual or entity that has a contract with a Managed Care Organization (MCO), Prepaid Inpatient Health Plan (PIHP), Prepaid Ambulatory Health Plan (PAHP), or Primary Care Case Manager (PCCM) entity that relates directly or indirectly to the performance of the MCO's, PIHP's, PAHP's, or PCCM entity's obligations under its contract with the State. Reference: Title 42 CFR 438.2A
Supportive housing: Supportive housing means housing with no limit on the length of stay that is occupied by the target population, and that is linked to onsite or offsite services that assist the supportive housing resident in retaining the housing, improving their health status, and maximizing their ability to live and, when possible, work in the community. References: W&I Code 5830(b)(2)(C); HSC 50675.14; HSC 50675.2(h)
Supportive Services: Supportive Services refers to services necessary to support individuals’ recovery and wellness, including, but not limited to, food, clothing, linkages to needed social services, linkages to programs administered by the federal Social Security Administration, vocational and education-related services, employment assistance, including supported employment, psychosocial rehabilitation, family engagement, psychoeducation, transportation assistance, occupational therapy provided by an occupational therapist, and group and individual activities that promote a sense of purpose and community participation. Reference: W&I Code 5887, subdivision (h)(3)
Underserved cultural populations: Underserved cultural populations refers to those who are unlikely to seek help from providers of traditional mental health and substance use disorder services because of stigma, lack of knowledge, or other barriers, including members of ethnically and racially diverse communities, members of the lesbian, gay, bisexual, transgender, queer and/or questioning (LGBTQ+) communities, victims of domestic violence and sexual abuse, and veterans, across their lifespans. Reference: W&I Code 5840.6, subdivision (f)(2)
Use by right: Use by right refers to a capital development project that satisfies both of the following conditions: (A) The development project does not require a conditional use permit, planned unit development permit, or other discretionary local government review. (B) The development project is not a “project” for purposes of Division 13 (commencing with Section 21000) of the Public Resources Code." Reference: W&I Code 5831, subdivision (e)(2)
[1] Licensure: CDSS
[2] Licensure: CDSS
[3] Licensure: CDSS
[4] Licensure: DHCS
[5] Licensure: CDSS
[6] Licensure: DHCS
[7] DHCS will seek to align the list of eligible settings under BHT and Transitional Rent to ensure seamless transitions between funding sources.
[8] All individual practitioners must be credentialed according to credentialing requirements stated in BHINs 18-019 and 22-070. The full list of providers and facilities eligible and required to enroll in Medi-Cal through PAVE is available on DHCS webpage “Provider Enrollment Options.” See also DHCS webpage Application Information by Provider Type. Providers apply for Medi-Cal enrollment with the Provider Enrollment Division. Almost all individual SMHS providers and facilities are required to enroll in Medi-Cal, as described in BHIN 20-071. DHCS’s SUD Licensing and Certification Toolkit outlines the full process for Medi-Cal certification and enrollment for DMC/DMC-ODS providers: “DHCS Level of Care Designation and ASAM Level of Care Certification.” SMHS certification and recertification requirements are outlined in 9 CCR § 1810.435,the Mental Health Plan: Certifications (MHP-owned & operated Clinics) materials and the current county SMHS contract with DHCS.
Unlike DMC/DMC-ODS providers, SMHS providers are permitted to contract with a BHP and begin claiming for Medi-Cal services while their certification is pending. SUD providers must become DMC certified before they can be county-contracted providers, as described in in W&I Code § 14124.24(e).
[9] W&I Code § 5891, subdivision (a)(3)(A)
[10] DMHC regulations require commercial health plan to reimburse claims from out of network providers at a “reasonable and customary value for the health care services rendered.” 28 CCR § 1300.71(a)(3)(B).
[11] H&S Code § 1367(h)(2) requires the commercial plan to implement these dispute resolution process for out of network providers.
[13] For example, lists of services that require prior authorization are available on the following plan websites or portals: Health Net, Anthem, Blue Shield (list of services requiring PA), Blue Shield (general instructions on submitting PA).
[14] Please see the definition in Appendix D.
[15] “Letter of agreement” means an agreement for reimbursement reflecting the terms and conditions of payment, including the payment amount, between a plan and provider for more than one episode of care for more than one patient, when the provider is out of network or the treatment is not covered under the patients’ plan.
[16] H&S Code § 1374.72; Ins. Code § 10144.5
[17] Eligible services and programs are outlined in the Legislative Analyst’s Office Report on 1991 Realignment. (October 2018). California Department of Social Services. (Updated May 2016). 2011 Realignment. Rethinking the 1991 Realignment. Legislative Analyst’s Office. (August 2011). 2011 Realignment: Addressing Issues to Promote Its Long-Term Success.
[18] Counties may have other resources from State General Funds that are not impacted by this policy; for example, counties are eligible to apply for grants through the Children and Youth Behavioral Health Initiative (CYBHI) and CYBHI is an investment using State General Funds.
[19] California Department of Health Care Services. (September 2023). California Opioid Settlements.
[20] California Department of Health Care Services. Community Mental Health Services Block Grant.
[21] DHCS outlines allowable use of SUBG, including prevention and perinatal set-aside requirements, in the SUBG Policy Manual. SUBG Policy Manual, Version 3.0 (5.21.2024).
[22] DHCS outlines use of SAMHSA PATH on their webpage.
